by Jason Wasserman MD PhD FRCPC
March 7, 2023
What is chronic colitis?
Chronic colitis is a condition where immune cells attack and damage the tissue that covers the inside of the colon. Chronic colitis is seen in inflammatory bowel disease including Crohn’s disease and ulcerative colitis.
What are the symptoms of chronic colitis?
Inflammation in the colon damages the cells that cover the inside of the colon. This prevents the colon from working normally. The damaged cells are unable to absorb water and patients with chronic colitis often experience diarrhea. Other symptoms of chronic colitis include abdominal pain, bloating, bloody stools, and weight loss.
What causes chronic colitis?
The most common cause of chronic colitis is inflammatory bowel disease (IBD). There are two types of inflammatory bowel disease, ulcerative colitis, and Crohn’s disease. Because both types of IBD can look similar when examined under the microscope, your pathologist may not be able to say whether the changes seen in your tissue sample are caused by ulcerative colitis or Crohn’s disease.
Your doctors will use the information in your pathology report along with other information they have collected (e.g. what they saw during the colonoscopy and other symptoms you have reported) to determine whether a diagnosis of a specific type of IBD can be made. Sometimes when inflammation is active, it can be difficult to differentiate between the two types of IBD.
How do pathologists make the diagnosis of chronic colitis?
If your doctor suspects that you have inflammation in your colon, they will perform a colonoscopy. A colonoscopy is a procedure where a small camera is used to see the inside of your colon. To determine whether inflammation is present, they will take tissue samples, called biopsies. Because chronic colitis can happen in one part of the colon but not another, they will likely take multiple biopsies from the entire length of the colon. Your pathologist will then examine these biopsies under a microscope to determine whether chronic colitis is present.
What does chronicity mean in a pathology report for chronic colitis?
When examining a biopsy from the colon, pathologists use the term chronicity to describe changes caused by long-standing or chronic inflammation. These changes include crypt distortion, basal lymphoplasmacytosis, and Paneth cell metaplasia. These changes are described in more detail in the sections below.
What does activity mean in a pathology report for chronic colitis?
When examining a biopsy from the colon, pathologists use the terms activity or active to describe tissue injury or damage caused by ongoing or acute inflammation. Pathologists often divide the activity into three levels – mild, moderate, and severe – based on the type of inflammation and damage seen in the tissue sample. Changes associated with activity or active colitis include cryptitis, crypt abscesses, and ulcers. These changes are described in more detail in the sections below.
What does quiescent colitis mean?
Patients who are receiving treatment for IBD will show signs of chronic colitis. Chronic colitis without ongoing damage or active colitis is called “quiescent colitis”. Another name for quiescent colitis is inactive colitis.
Changes associated with chronicity
Crypt distortion
The inside surface of the colon is covered by long test tube-shaped glands called crypts. Pathologists use the word distortion to describe changes in the size and shape of the crypts compared to normal. Crypt distortion is considered a sign of long-term damage. This means that crypt distortion is only seen when inflammation has been present for months or years.
Crypt architectural distortion can include the following:
- Atrophy – Atrophy is a loss of tissue compared to normal. In the colon, atrophy means that the crypts that are seen are smaller than normal, healthy crypts.
- Crypt loss – There is a complete loss of crypts in some areas of the mucosa.
- Branching – Instead of being long and straight, these crypts split to form multiple branches.

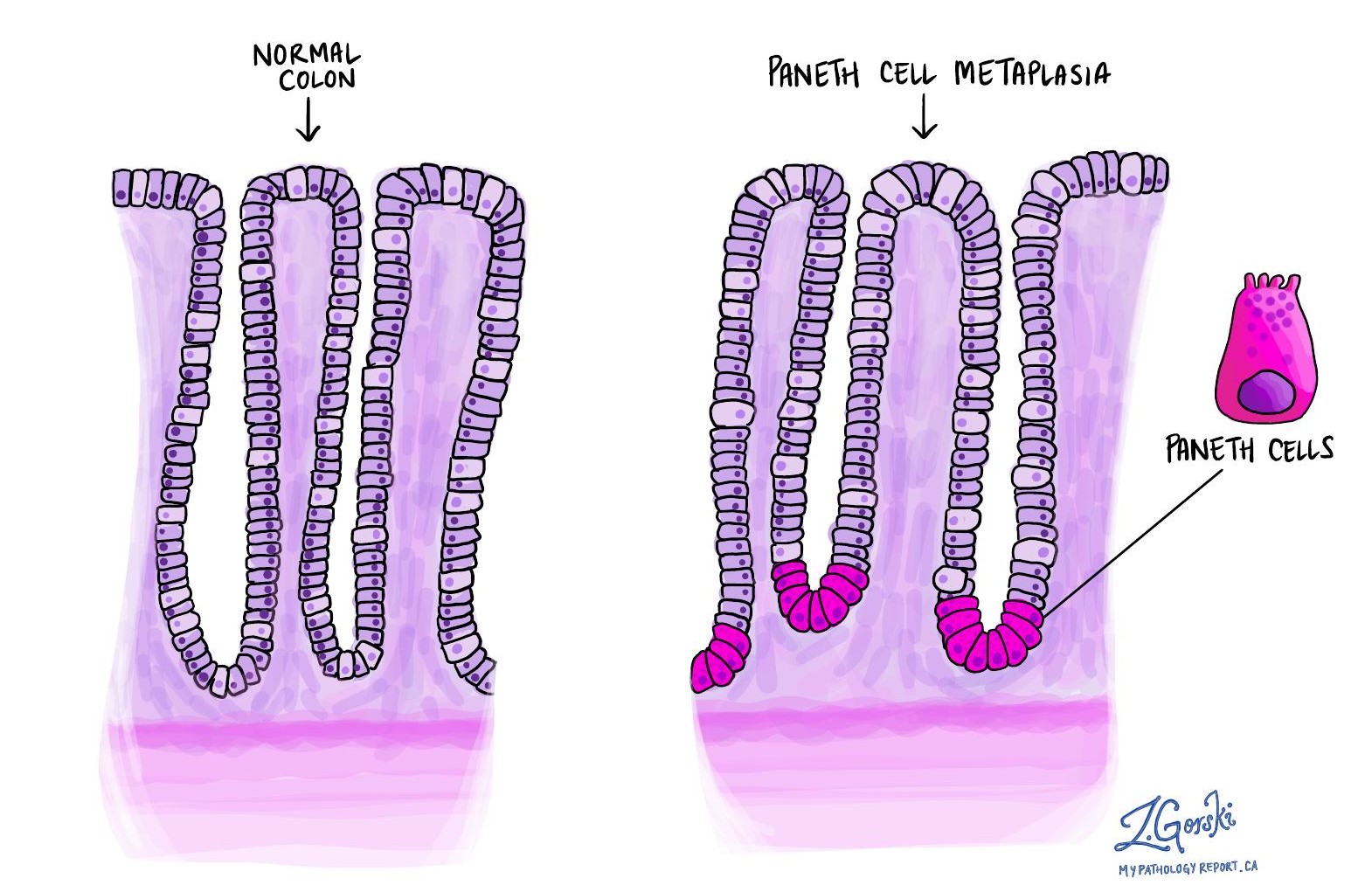
Paneth cell metaplasia
Paneth cells are a normal part of the digestive tract. They are usually found in the small intestine and the right side of the colon. However, if your pathologist sees Paneth cells in the tissue sample from the left side of your colon, they describe it as Paneth cell metaplasia. This is an abnormal finding that means that there is chronic damage to the mucosa of your colon. Paneth cell metaplasia is considered a sign of long-term damage. It is only seen when inflammation has been present for months or years.
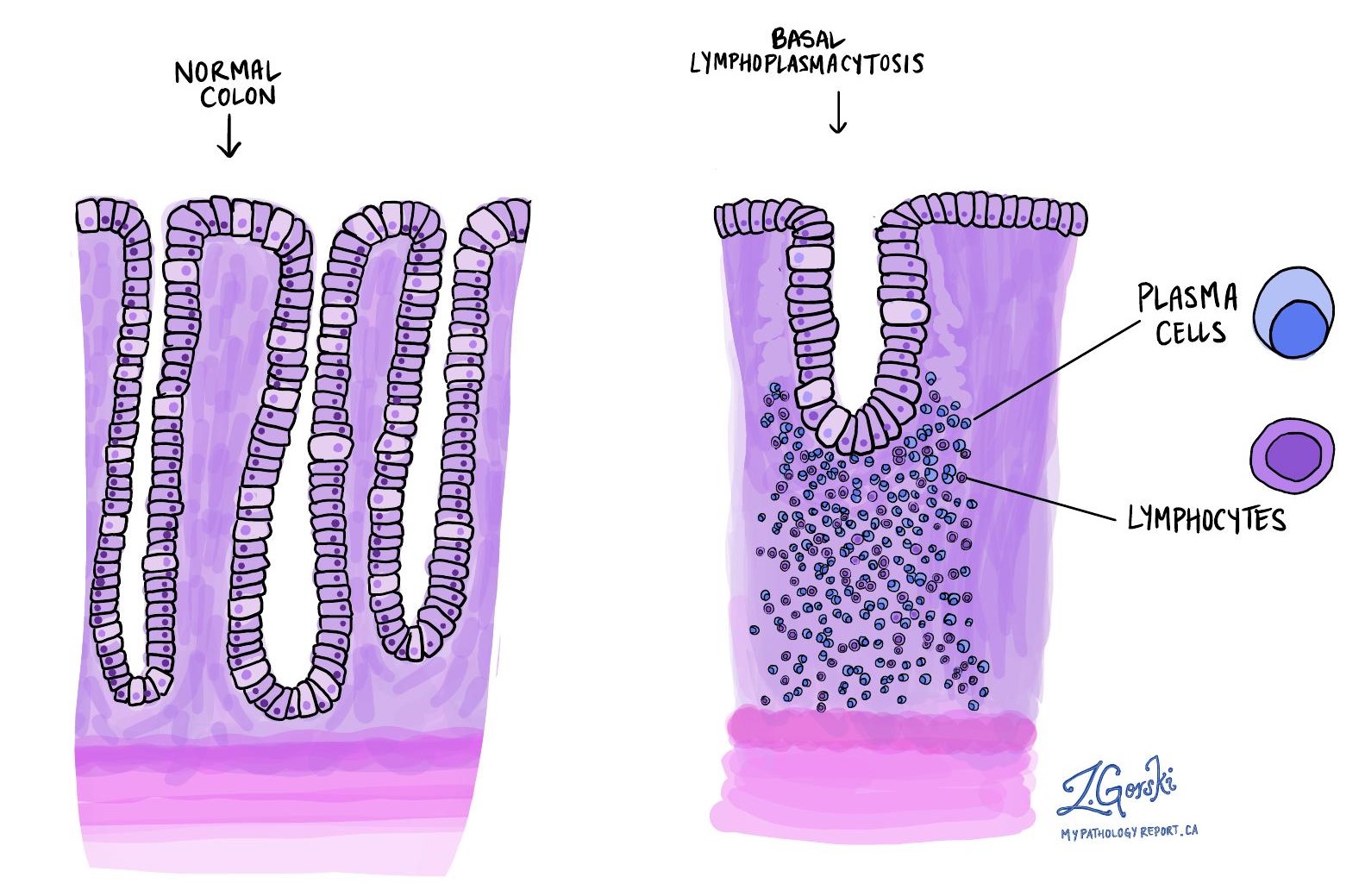
Basal lymphoplasmacytosis
Lymphocytes and plasma cells are specialized immune cells that help protect the body against infection. Large numbers of lymphocytes and plasma cells are not normally seen in a healthy colon. Basal lymphoplasmacytosis is a term pathologists use to describe a large number of lymphocytes and plasma cells in the mucosa surrounding the crypts. If your pathologist sees too many of these types of cells compressing and shortening the crypts, it means that the immune system is not working properly. Basal lymphoplasmacytosis is considered a sign of long-term damage. It is only seen when inflammation has been present for months or years.
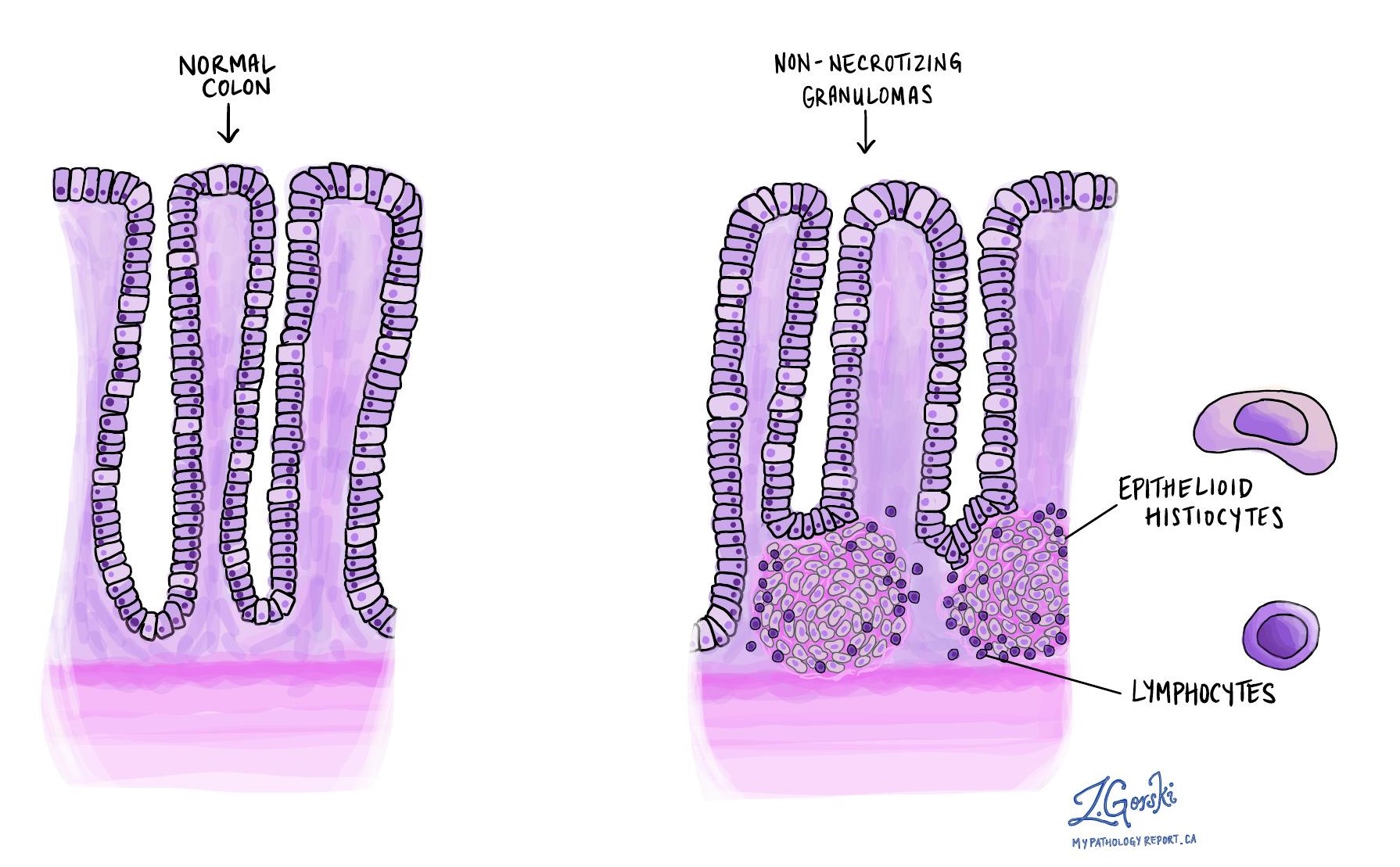
Granulomas
A granuloma is an organized collection of immune cells. Granulomas are a sign of chronic colitis. Their presence suggests that the condition is caused by Crohn’s disease rather than ulcerative colitis (where granulomas are rarely seen). The immune cells at the center of the granuloma are called histiocytes and they often join together to form giant cells. Some granulomas have an outer layer of lymphocytes, another specialized type of immune cell that works together with histiocytes.
Changes associated with activity
Cryptitis
Cryptitis is a word pathologists use to describe active or ongoing inflammation in the colon. Active inflammation is the body’s first defense response to injury or disease and is led by specialized immune cells called neutrophils. When neutrophils attack the body’s crypts, it is called cryptitis.
Cryptitis can be seen at the very early stages of the disease before other features of long-term damage develop (e.g., crypt distortion, basal lymphoplasmacytosis, and Paneth cell metaplasia). In patients with IBD, it can also mean that the treatments being used are not working.
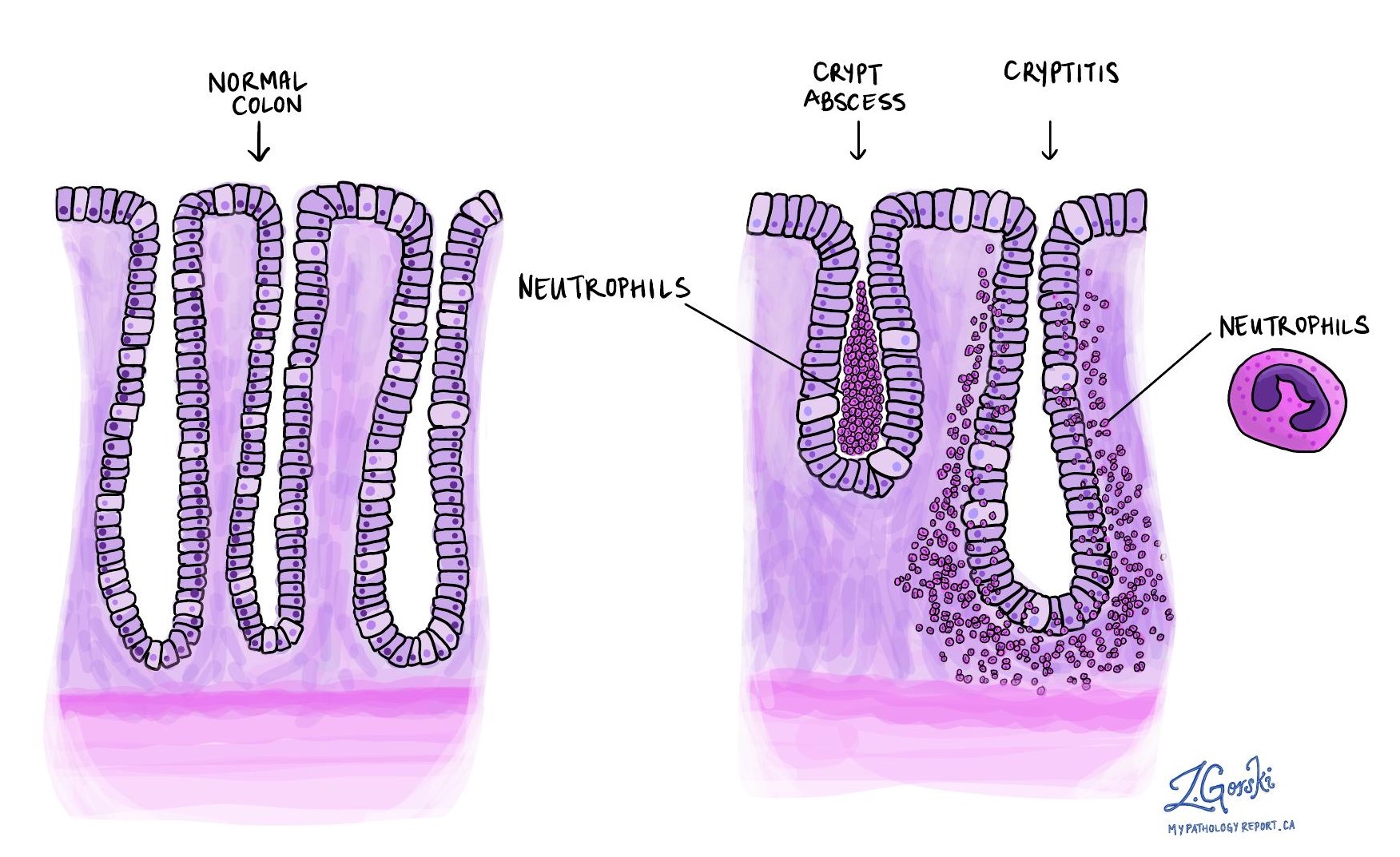
Crypt abscess
Crypt abscess is another term pathologists use to describe active or ongoing inflammation in the colon. It is a collection of neutrophils that are seen in the middle of the crypt (i.e. inside the test tube). Crypt abscesses can be seen at the very early stages of the disease before other features of long-term damage develop (e.g., crypt distortion, basal lymphoplasmacytosis, and Paneth cell metaplasia). In patients with IBD, it can also mean that the treatments being used are not working.
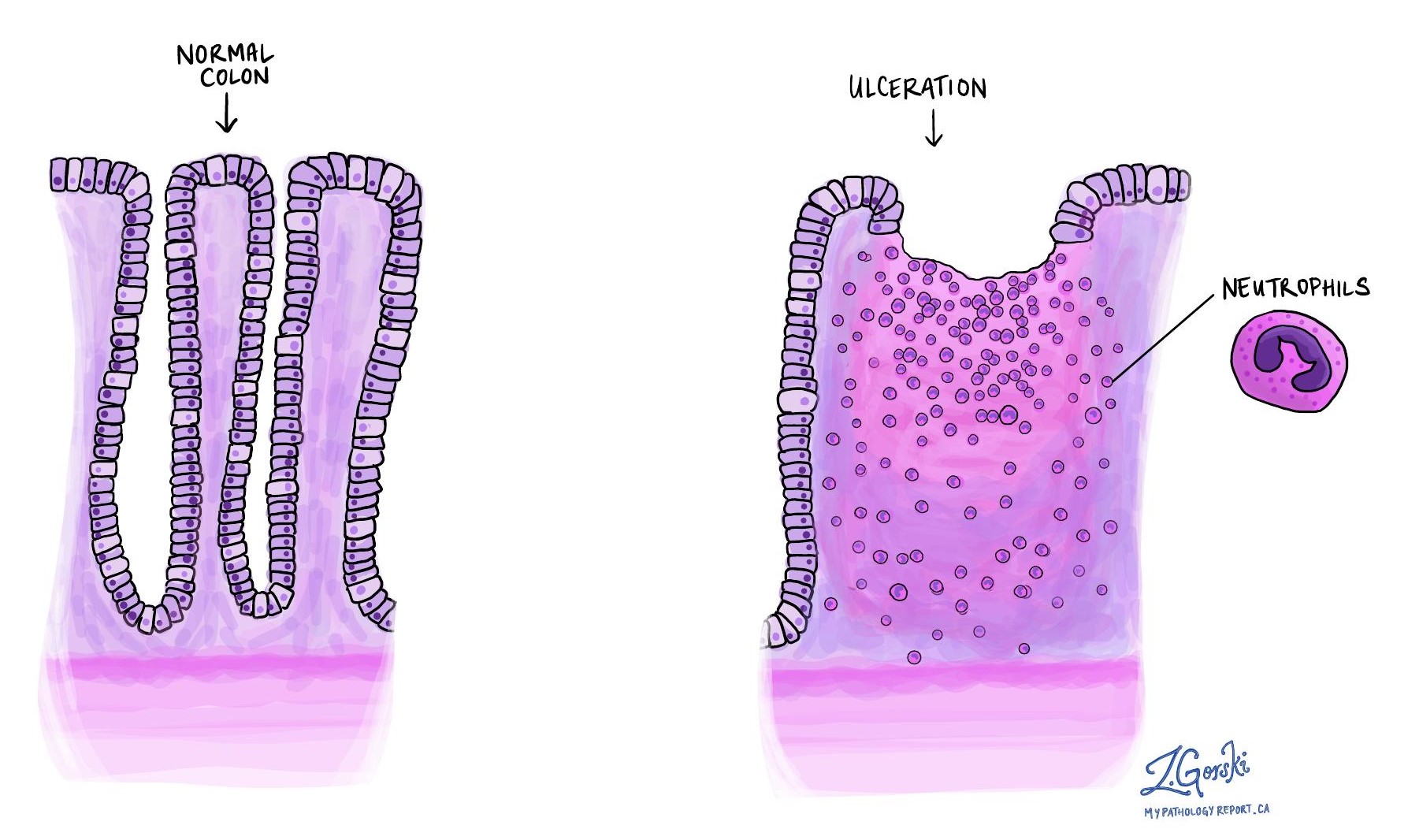
Ulceration
Ulceration describes severe damage associated with a complete loss of the inner layer of the colon (the mucosa). It is a sign that inflammation is causing ongoing damage to the colon. Ulceration can be seen at the very early stages of the disease before other features of long-term damage develop (e.g., crypt distortion, basal lymphoplasmacytosis, and Paneth cell metaplasia). In patients with IBD, it can also mean that the treatments being used are not working. It is more common in ulcerative colitis, but it can also be seen in Crohn’s disease.