by Jason Wasserman MD PhD FRCPC
January 17, 2024
Medullary carcinoma is a rare type of colon cancer. It is considered a subtype of adenocarcinoma. Compared to other types of colon cancer, medullary carcinoma is associated with a good prognosis. Despite their similar names, medullary carcinoma of the colon is not related to medullary carcinoma of the thyroid gland.
This article will help you understand your diagnosis and pathology report for medullary carcinoma of the colon.
What are the symptoms of medullary carcinoma of the colon?
The symptoms of medullary carcinoma depend on the location of the tumour within the colon. Tumours in the left colon (descending colon) or rectum can cause changes in bowel habits, bloody stools, abdominal pain, or bloating. Tumours in the right colon (ascending colon) may not cause any symptoms until the tumour is very large or has spread to other parts of the body.
What causes medullary carcinoma of the colon?
At present, we do not fully understand what causes a person to develop medullary carcinoma of the colon. However, this type of cancer is much more common in people with Lynch syndrome and the tumour cells often show a loss of normal DNA mismatch repair proteins. Alterations in the BRAF gene are also common and may contribute to the development of this type of cancer.
Where does medullary carcinoma of the colon start?
Medullary carcinoma of the colon starts from epithelial cells on the inside surface of the colon. These epithelial cells normally connect to form structures called glands. The glands together with the lamina propria and muscularis mucosae form a thin layer of tissue called the mucosa.

How is this diagnosis made?
The diagnosis of medullary carcinoma is usually made after a small tissue sample is removed during an examination called a colonoscopy. The procedure used to remove the tissue may be called a biopsy or polypectomy. The tissue sample is then sent to a pathologist for examination under the microscope. The diagnosis can also be made after the entire tumour is removed along with a portion of the normal colon in a procedure called a colectomy.
Your pathology report for medullary carcinoma of the colon
The information found in your pathology report for medullary carcinoma of the colon will depend on the type of procedure performed. For example, the information found in a report after a biopsy is performed is usually limited to the diagnosis although some reports may also describe the results of additional tests such as mismatch repair proteins (see section below for more information). After the entire tumour has been removed, your pathology report will include additional information such as the tumour grade, level of invasion, presence or absence of lymphovascular and perineural invasion, and the assessment of margins. The results of any lymph nodes examined should also be included in this final report. These topics are described in more detail in the sections below.
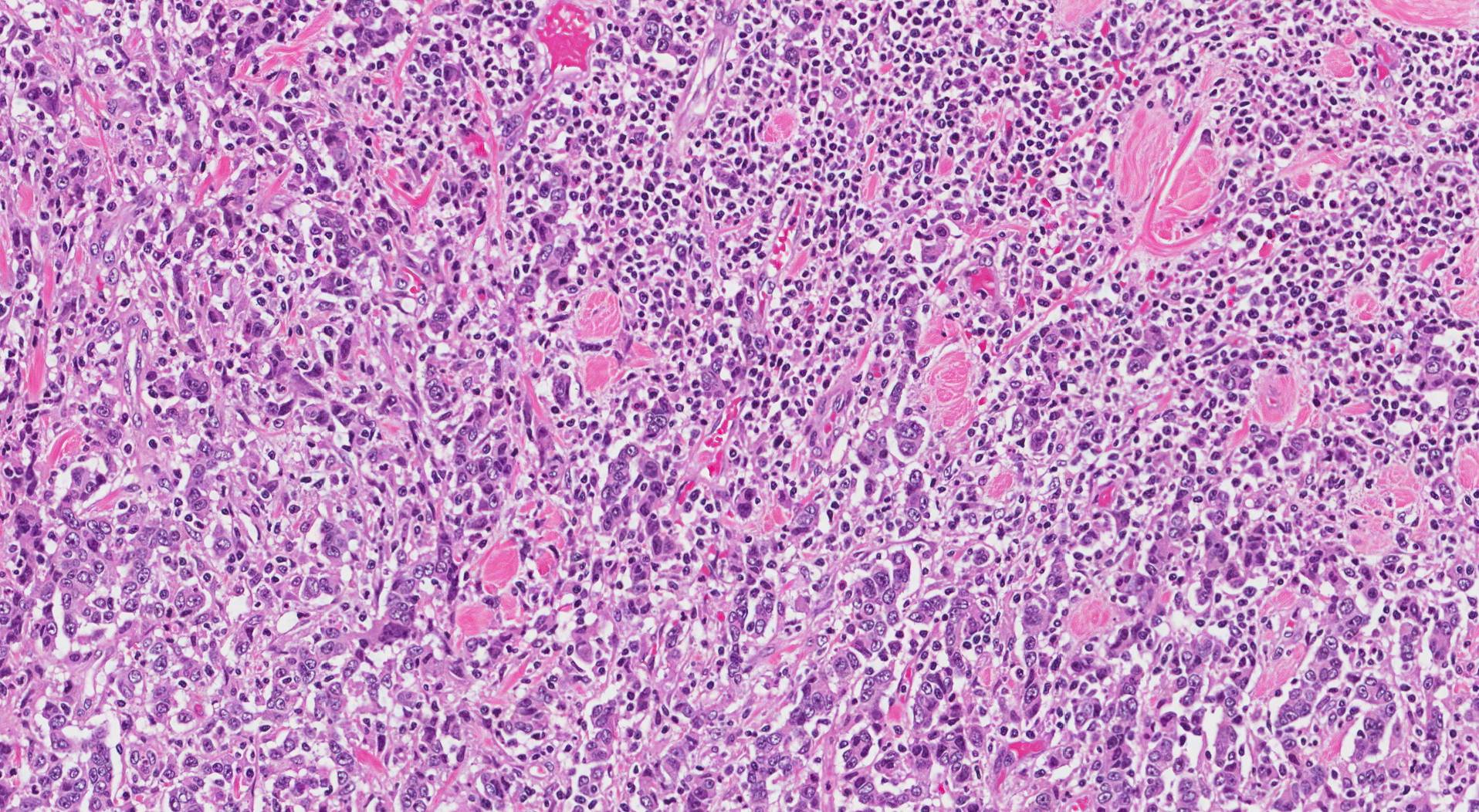
Microscopic features
When examined under the microscope, medullary carcinoma of the colon is made up of large tumour cells connected in groups called sheets. The tumour cells do not form glands (the structures normally found in the colon). The nucleus of the tumour cell (the part of the cell that holds the genetic material) is often large and round and clumps of genetic material called nucleoli are often seen. As the tumour grows it pushes into the surrounding normal colon (pathologists often describe this as a “pushing border”) and immune cells called lymphocytes are often seen throughout the tumour. When a test called immunohistochemistry is performed, the tumour cells typically show a loss of normal colonic markers such as cytokeratin 20 (CK20) and CDX-2.
What does it mean if the tumour is described as poorly differentiated?
In pathology, the term differentiated is used when comparing a tumour with normal, healthy cells. Medullary carcinoma is described as poorly differentiated because, unlike the normal, healthy cells in the colon, it does not form any round structures called glands.
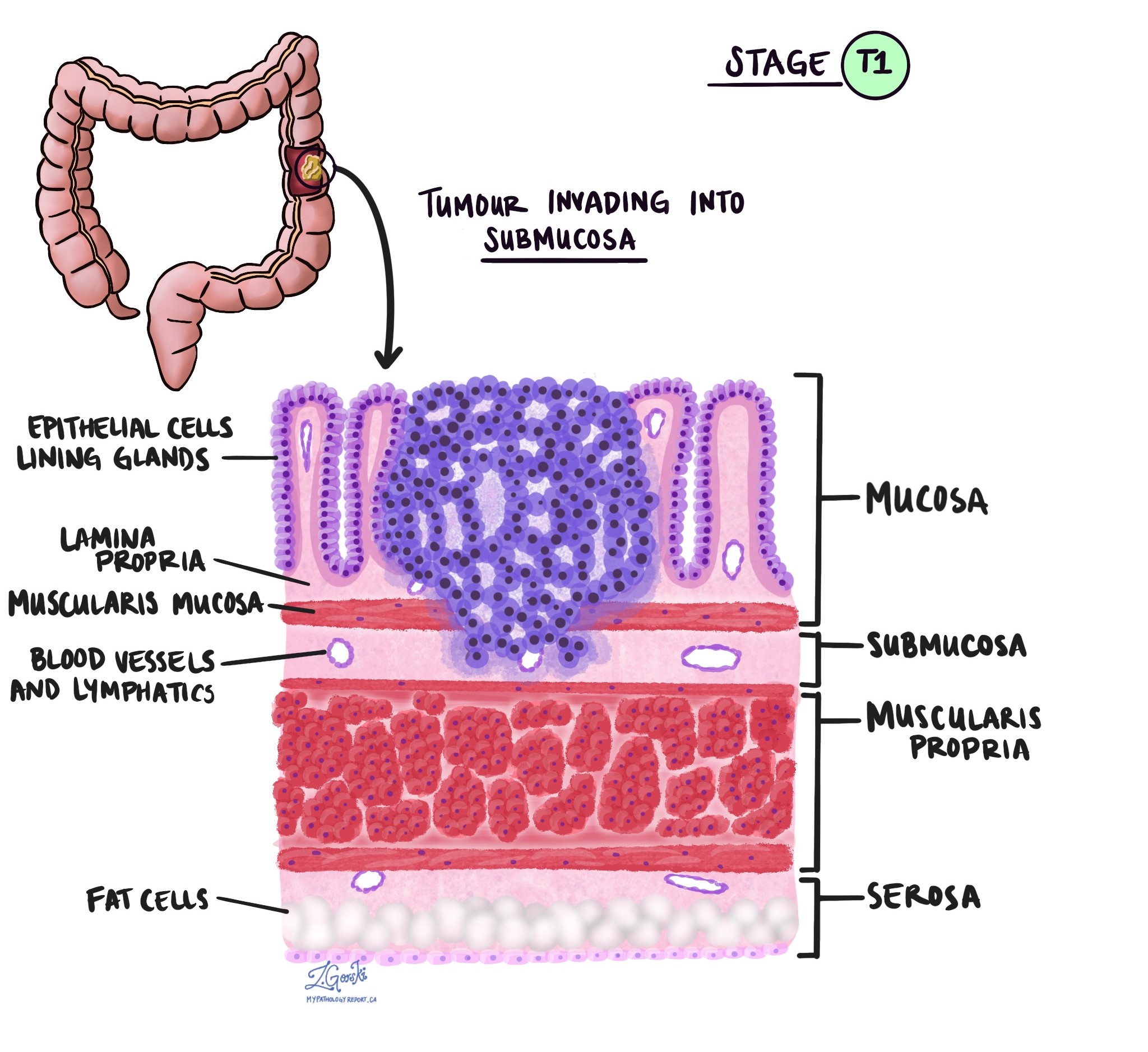
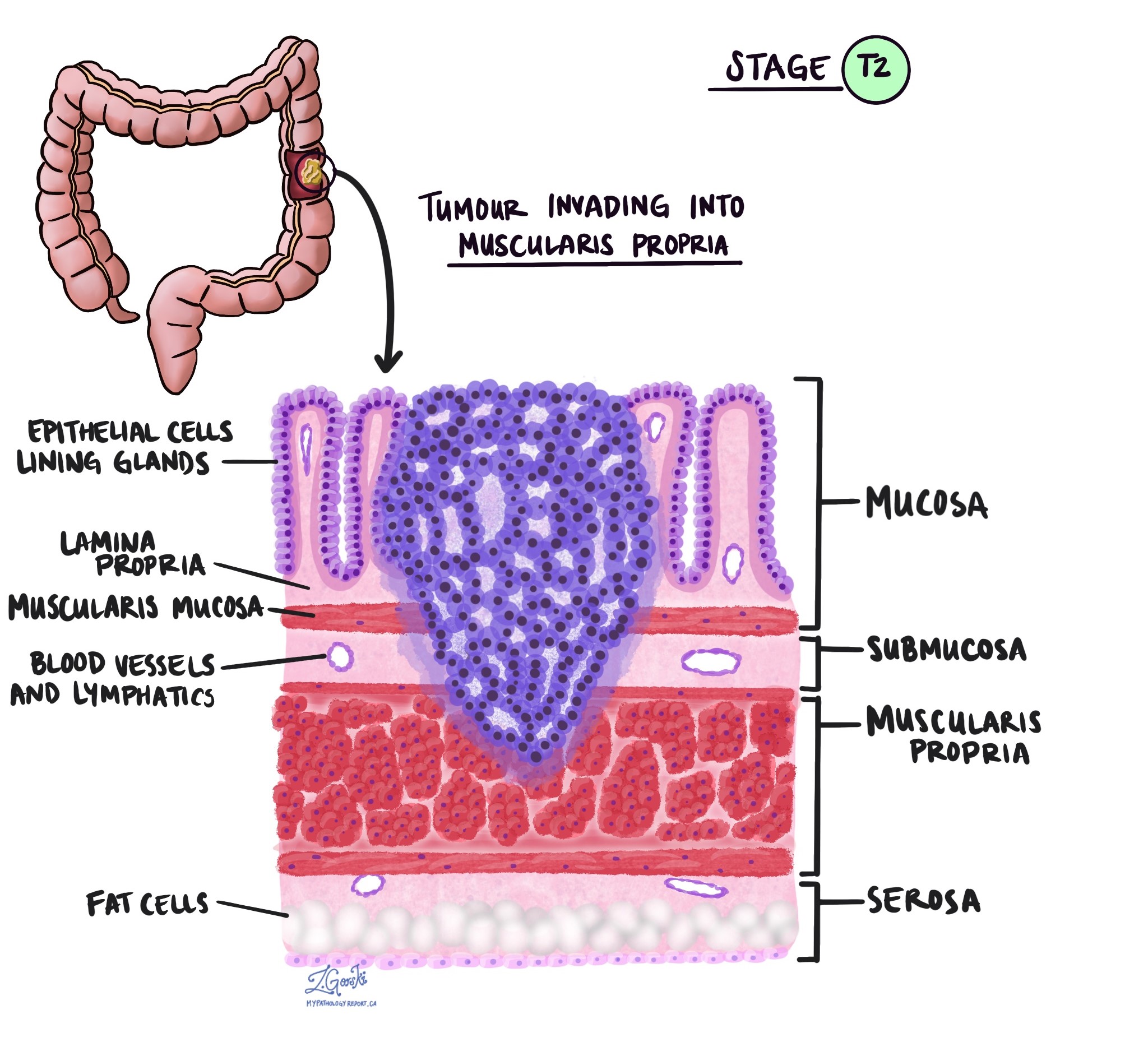
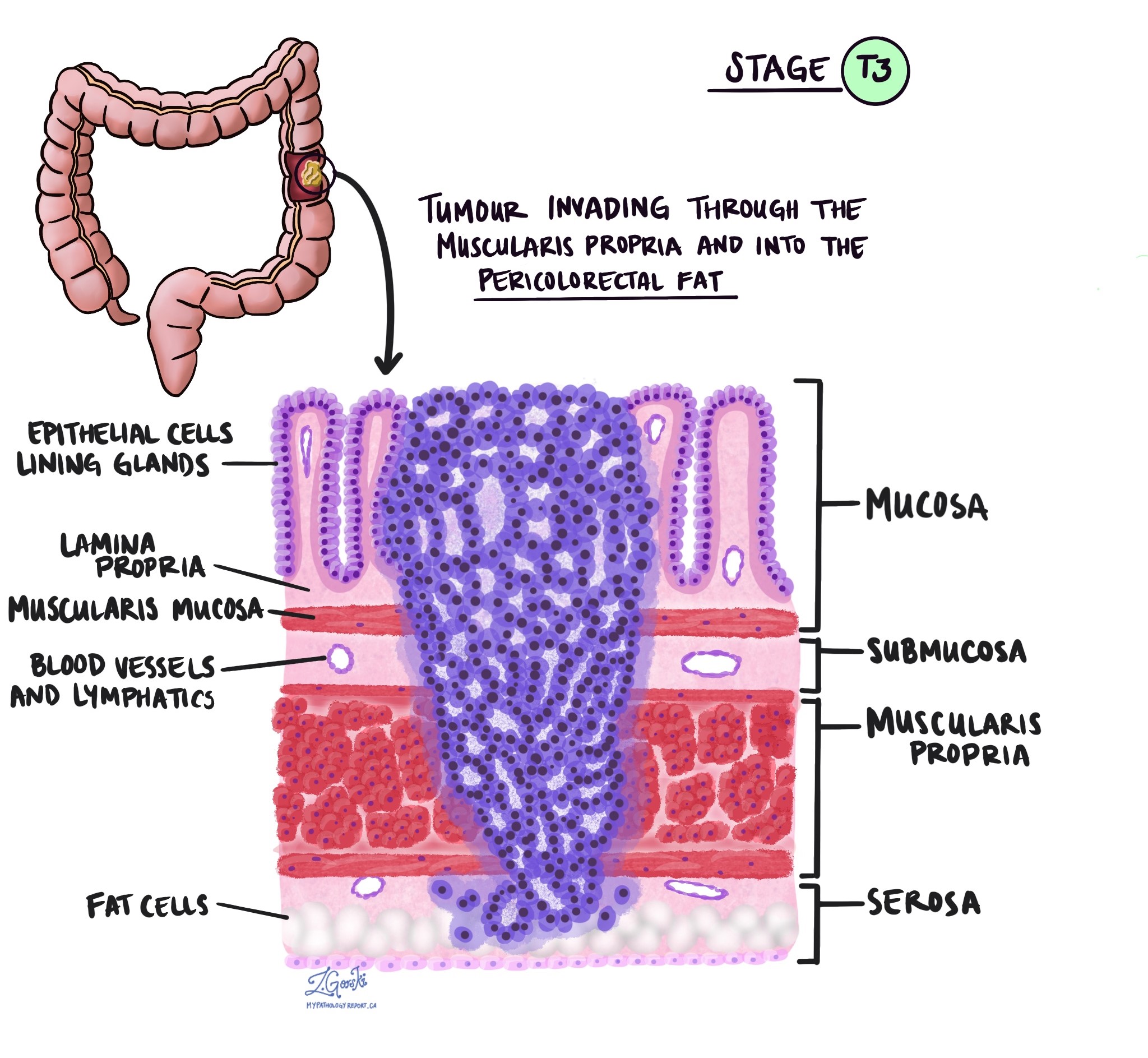
Depth of invasion
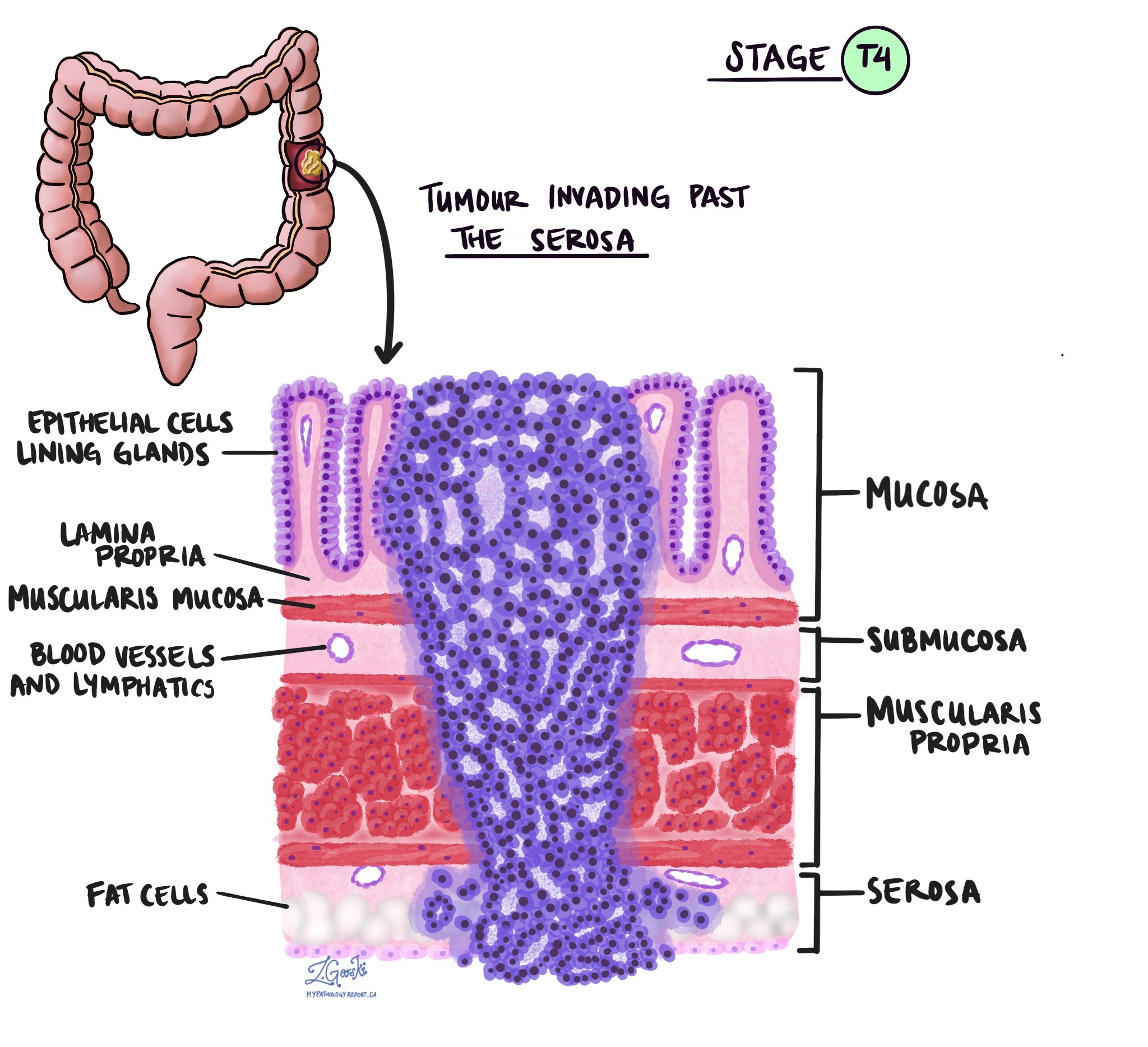
In pathology, the term invasion is used to describe the spread of cancer cells into organs or tissues surrounding the location where the tumour started. Because medullary carcinoma starts in a thin layer of tissue on the inside surface of the colon called the mucosa, invasion is defined as the spread of cancer cells into the other layers of tissue in the colon or any other organs outside of the colon. Invasion can only be seen after the tumour has been examined under a microscope by a pathologist.
When examining the tumour under the microscope, your pathologist will look to see how far the cancer cells have spread from the mucosa into the surrounding tissue. This is called the level of invasion. The level of invasion is important because tumours that invade deeper into the wall of the colon are more likely to spread to other parts of the body such as lymph nodes, the liver, or the lungs. The level of invasion is also used to determine the pathologic tumour stage (pT).
Perineural invasion
Pathologists use the term “perineural invasion” to describe a situation where cancer cells attach to or invade a nerve. “Intraneural invasion” is a related term that specifically refers to cancer cells found inside a nerve. Nerves, resembling long wires, consist of groups of cells known as neurons. These nerves, present throughout the body, transmit information such as temperature, pressure, and pain between the body and the brain. The presence of perineural invasion is important because it allows cancer cells to travel along the nerve into nearby organs and tissues, raising the risk of the tumour recurring after surgery.

Lymphovascular invasion
Lymphovascular invasion occurs when cancer cells invade a blood vessel or lymphatic channel. Blood vessels, thin tubes that carry blood throughout the body, contrast with lymphatic channels, which carry a fluid called lymph instead of blood. These lymphatic channels connect to small immune organs known as lymph nodes, scattered throughout the body. Lymphovascular invasion is important because it enables cancer cells to spread to other body parts, including lymph nodes or the liver, via the blood or lymphatic vessels. The presence of cancer cells inside a large vein past beyond the wall of the colon (outside of the thick bundle of muscle) is associated with a high risk that the cancer cells will eventually be found in the liver.

Margins
In pathology, a margin refers to the edge of tissue removed during tumour surgery. The margin status in a pathology report is important as it indicates whether the entire tumour was removed or if some was left behind. This information helps determine the need for further treatment.
Pathologists typically assess margins following a surgical procedure like an excision or resection, aimed at removing the entire tumour. Margins aren’t usually evaluated after a biopsy, which removes only part of the tumour. The number of margins reported and their size—how much normal tissue is between the tumour and the cut edge—vary based on the tissue type and tumour location.
Pathologists examine margins to check if tumour cells are present at the tissue’s cut edge. A positive margin, where tumour cells are found, suggests that some cancer may remain in the body. In contrast, a negative margin, with no tumour cells at the edge, suggests the tumour was fully removed. Some reports also measure the distance between the nearest tumour cells and the margin, even if all margins are negative.

Treatment effect
If you received treatment (either chemotherapy or radiation therapy or both) for your cancer before the tumour is removed, your pathologist will carefully examine the area of the tissue where the tumour was previously identified to see if any cancer cells are still alive (viable). The most commonly used system describes the treatment effect on a scale of 0 to 3 with 0 being no viable cancer cells (all the cancer cells are dead) and 3 being extensive residual cancer with no apparent regression of the tumour (all or most of the cancer cells are alive).
Tumour deposit
A tumour deposit is a group of cancer cells that are separate from the main tumour but not in a lymph node. Tumour deposits are associated with a higher risk that the tumour cells will spread to another part of the body such as the liver or lungs after treatment. Tumour deposits are also used to determine the pathologic tumour stage (pT).
Lymph nodes
Lymph nodes are small immune organs found throughout the body. Cancer cells can spread from a tumour to lymph nodes through small lymphatic vessels. For this reason, lymph nodes are commonly removed and examined under a microscope to look for cancer cells. The movement of cancer cells from the tumour to another part of the body such as a lymph node is called a metastasis.
Cancer cells typically spread first to lymph nodes close to the tumour although lymph nodes far away from the tumour can also be involved. For this reason, the first lymph nodes removed are usually close to the tumour. Lymph nodes further away from the tumour are only typically removed if they are enlarged and there is a high clinical suspicion that there may be cancer cells in the lymph node.
If any lymph nodes were removed from your body, they will be examined under the microscope by a pathologist and the results of this examination will be described in your report. “Positive” means that cancer cells were found in the lymph node. “Negative” means that no cancer cells were found. If cancer cells are found in a lymph node, the size of the largest group of cancer cells (often described as “focus” or “deposit”) may also be included in your report. Extranodal extension means that the tumour cells have broken through the capsule on the outside of the lymph node and have spread into the surrounding tissue.
The examination of lymph nodes is important for two reasons. First, this information is used to determine the pathologic nodal stage (pN). Second, finding cancer cells in a lymph node increases the risk that cancer cells will be found in other parts of the body in the future. As a result, your doctor will use this information when deciding if additional treatment such as chemotherapy, radiation therapy, or immunotherapy is required.

Mismatch repair proteins
Mismatch repair (MMR) is a system inside all normal, healthy cells for fixing mistakes in our genetic material (DNA). The system is made up of different proteins and the four most common are called MSH2, MSH6, MLH1, and PMS2.
The four mismatch repair proteins MSH2, MSH6, MLH1, and PMS2 work in pairs to fix damaged DNA. Specifically, MSH2 works with MSH6 and MLH1 works with PMS2. If one protein is lost, the pair cannot function normally. A loss of one of these proteins increases the risk of developing cancer.
Pathologists order mismatch repair testing to see if any of these proteins are lost in a tumour. If mismatch repair testing has been ordered on your tissue sample, the results will be described in your pathology report.
Why is testing for mismatch repair proteins important?
Mismatch repair (MMR) testing is performed on colon cancers to identify patients who may have Lynch syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC). Lynch syndrome is a genetic disorder that increases the risk of developing various types of cancer, including colon cancer, endometrial cancer, ovarian cancer, gastric cancer, and others.
How do pathologists test for mismatch repair proteins?
The most common way to test for mismatch repair proteins is to perform a test called immunohistochemistry. This test allows pathologists to see if the tumour cells are producing all four mismatch repair proteins. A normal result will say that the protein is retained or expressed. An abnormal result will say that there is a loss of the protein or that the protein is deficient.
Pathologic stage
The pathologic stage for medullary carcinoma of the colon is based on the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer. This system uses information about the primary tumour (T), lymph nodes (N), and distant metastatic disease (M) to determine the complete pathologic stage (pTNM). Your pathologist will examine the tissue submitted and give each part a number. In general, a higher number means a more advanced disease and a worse prognosis.
The pathologic stage is not reported on a biopsy specimen. It is only reported when the entire tumour has been removed in an excision or resection specimen.
Tumour stage (pT)
Medullary carcinoma of the colon is given a tumour stage between 1 and 4 based on the depth of invasion (the distance the cancer cells have spread from the mucosa into the wall of the colon or surrounding tissues).
- T1 – The cancer cells have spread into the submucosa just below the mucosa on the inner surface of the colon.
- T2 – The cancer cells have spread into the muscularis propria of the colon.
- T3 – The cancer cells have spread into fat near the outer surface of the colon.
- T4 – The cancer cells have spread into a layer of tissue called the serosa on the outer surface of the colon or the cancer cells have spread into surrounding organs such as the bladder or abdominal wall.
Nodal stage (pN)
Medullary carcinoma of the colon is given a nodal stage between 0 and 2 based on whether any cancer cells were found in any of the lymph nodes examined or the finding of tumour deposits. If no cancer cells were found in any of the lymph nodes examined, the nodal stage is N0. If no lymph nodes were sent for pathologic examination, the nodal stage cannot be determined and is listed as NX.
About this article
This article was written by medical doctors in conjunction with patient advisers. It was designed to help patients read and understand their pathology report for medullary carcinoma of the colon. The sections above explain many of the most common features found in pathology reports for this condition. If you have any questions about this article, please contact us.



