by Catherine Forse MD FRCPC
July 21, 2025
Microscopic colitis is a non-cancerous condition that affects the colon, a part of the large intestine. It occurs when certain immune cells accumulate in the inner lining of the colon, resulting in inflammation and tissue damage. This inflammation interferes with the colon’s ability to absorb water, which can result in persistent watery diarrhea. The condition is called “microscopic” because the colon often looks normal during a colonoscopy, and the inflammation can only be seen when the tissue is examined under a microscope.
There are two main types of microscopic colitis:
What are the symptoms of microscopic colitis?
People with microscopic colitis often experience:
-
Chronic watery diarrhea, which may last for weeks, months, or even years.
-
Abdominal cramping or pain.
-
Unintentional weight loss.
-
Fatigue or tiredness.
Because the symptoms can overlap with other digestive conditions, microscopic colitis may take time to diagnose.
What causes microscopic colitis?
The exact cause of microscopic colitis is still not fully understood. However, researchers believe several factors may contribute to the development of this condition:
-
Autoimmune response: Some scientists think the body’s immune system may mistakenly attack the cells in the colon, leading to inflammation.
-
Response to substances in the colon: Another theory suggests that the condition could be triggered by bacteria, medications, or toxins present in stool.
-
Other contributing factors: Genetics, smoking, and certain medications (such as nonsteroidal anti-inflammatory drugs or proton pump inhibitors) may increase the risk.
More research is needed to fully understand what causes microscopic colitis and why it affects some people but not others.
How is the diagnosis of microscopic colitis made?
Because the inflammation in microscopic colitis is not visible to the naked eye, the diagnosis requires a biopsy. If your doctor suspects microscopic colitis based on your symptoms, they will likely recommend a colonoscopy. This is a procedure that uses a small camera to view the inside of the colon. During the procedure, small tissue samples (biopsies) will be taken from different parts of the colon.
The tissue is then sent to a pathologist, who examines it under a microscope to look for signs of inflammation. Since the changes in microscopic colitis can affect some areas of the colon more than others, it is important to take multiple biopsies from throughout the colon.
For most patients, the colon will look normal during the colonoscopy. That is why a microscopic examination of the tissue is essential to make the diagnosis.
What are the types of microscopic colitis?
Pathologists divide microscopic colitis into two types based on the features seen under the microscope: lymphocytic colitis and collagenous collagenous colitis. Both types are explained in greater detail in the sections below.
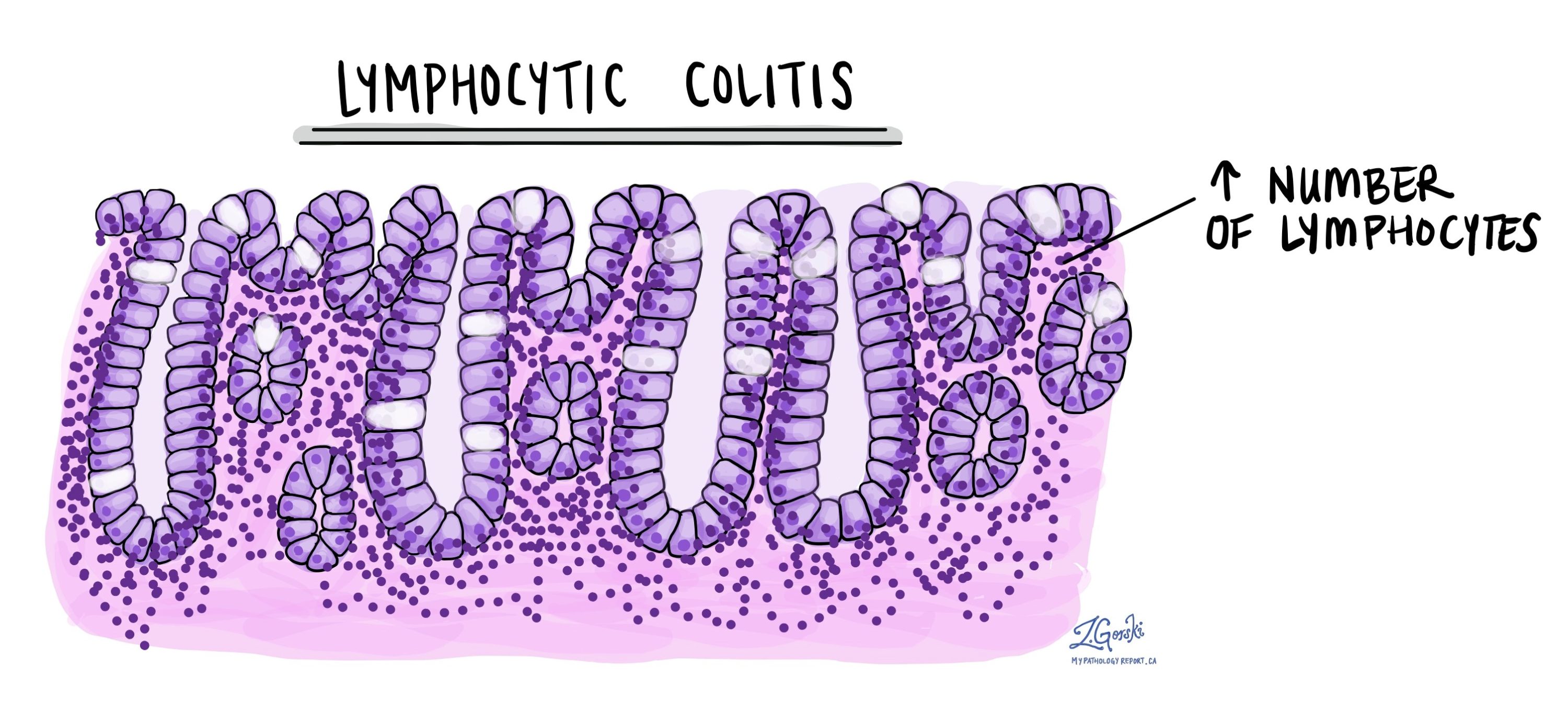
Lymphocytic colitis
In lymphocytic colitis, there is an increased number of immune cells called lymphocytes within the mucosa (inner lining) of the colon. These lymphocytes are found both within the glands (also called crypts) and in the surrounding tissue known as the lamina propria. This pattern is called intraepithelial lymphocytosis.
Over time, the increased number of lymphocytes can damage the lining of the colon. The glands may become smaller and less functional, a process called atrophy. Damaged glands produce less mucin, which is a substance that helps protect and lubricate the colon. This damage may reduce the colon’s ability to absorb water properly, leading to diarrhea.
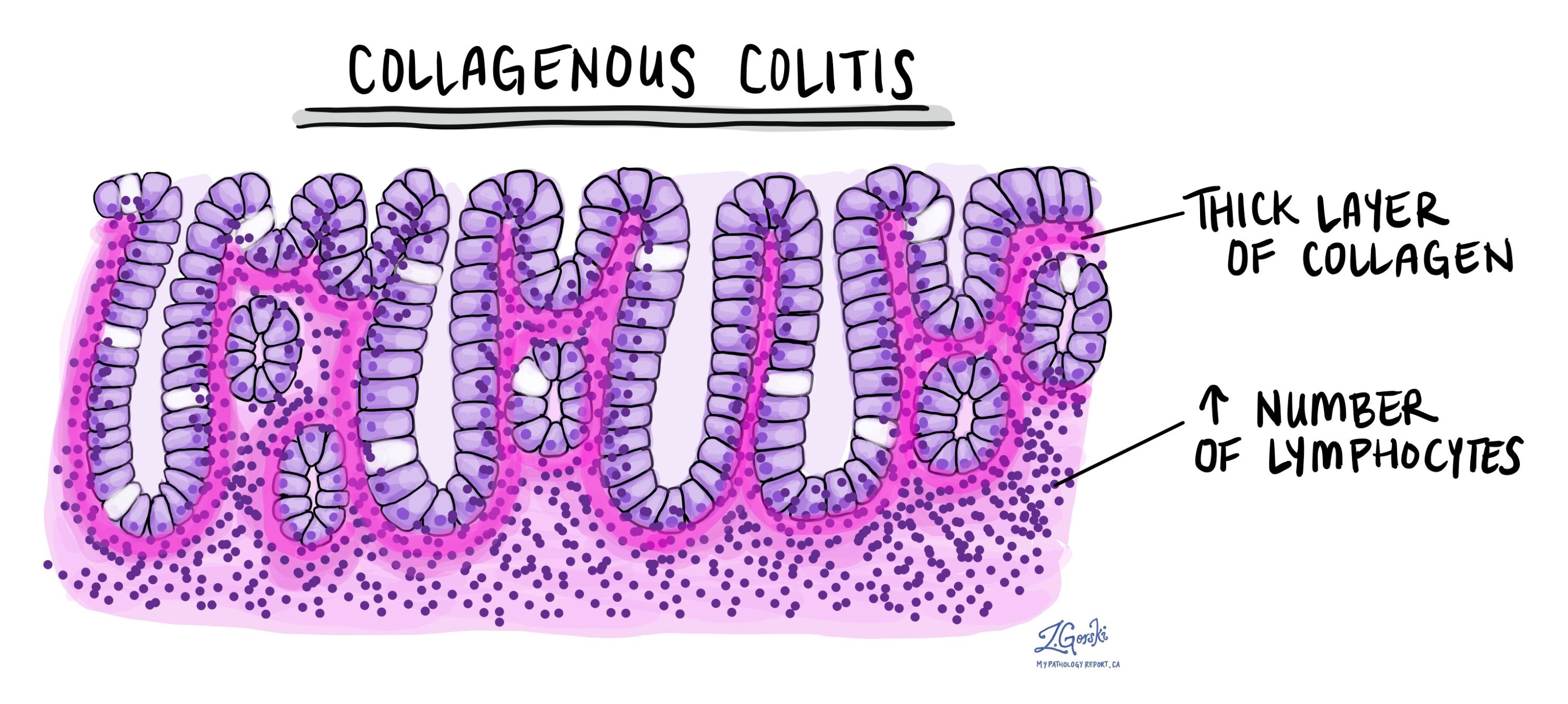
Collagenous colitis
Collagenous colitis has many of the same features as lymphocytic colitis, including an increased number of lymphocytes and signs of epithelial cell damage. However, collagenous colitis has an additional feature: a thickened layer of collagen (a type of structural protein) beneath the surface lining of the colon. This thick layer separates the epithelium from the lamina propria and can be seen as a pink band when viewed under a microscope.
This abnormal collagen layer may trap small blood vessels and immune cells near the surface and interfere with the colon’s normal function. The extra collagen is thought to be produced by overactive support cells called myofibroblasts. In some cases, pathologists may use a special stain called Masson’s trichrome to highlight the collagen band and confirm the diagnosis.
Is microscopic colitis the same as inflammatory bowel disease (IBD)?
No. While both microscopic colitis and inflammatory bowel disease (IBD) cause chronic inflammation in the colon, they are different conditions with different microscopic features. In IBD, the shape and structure of the glands in the colon are often distorted or irregular (a change called crypt distortion), and inflammation usually affects deeper layers of the colon wall. These changes are not typically seen in microscopic colitis.
To learn more about IBD, see our article on chronic colitis.
Questions to ask your doctor
-
What type of microscopic colitis do I have—lymphocytic or collagenous?
-
What treatment options are available to manage my symptoms?
-
Are there any medications I should avoid that could make the condition worse?
-
Will I need follow-up colonoscopies or repeat biopsies?
- Is microscopic colitis linked to any long-term health risks?
-
Should I consider seeing a specialist, such as a gastroenterologist?


