by Emily Goebel, MD FRCPC
January 12, 2023
What is an endometrial polyp?
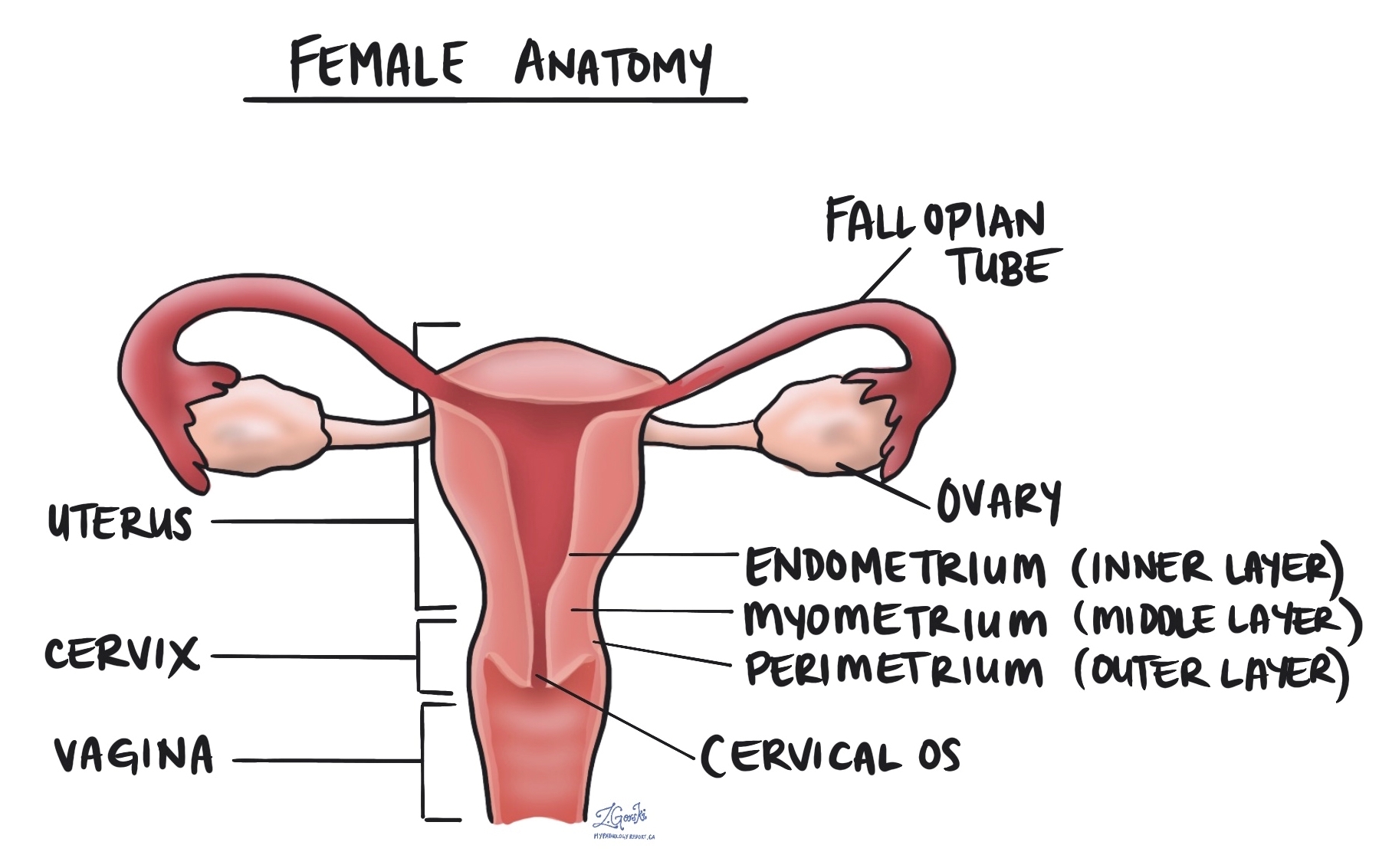
An endometrial polyp is a non-cancerous growth found on the inside of the uterus. The polyp sticks out from the thin layer of tissue on the inside uterus called the endometrium. The polyp is made up of an increased number of otherwise normal-appearing endometrial glands and stroma.
What causes an endometrial polyp?
The growth and development of the normal endometrium are controlled by hormones such as estrogen. High levels of estrogen can cause increased growth of the tissue in the endometrium and over time the development of an endometrial polyp. Other associated conditions include high blood pressure, obesity, late menopause, and tamoxifen treatment.
What are the symptoms of an endometrial polyp?
The most common symptoms associated with endometrial polyps are post-menopausal or abnormal vaginal bleeding. Some patients will not experience any symptoms and the polyp will be discovered during a medical procedure for another condition.
How is the diagnosis of endometrial polyp made?
In patients with abnormal vaginal bleeding, the endometrium is usually sampled by endometrial biopsy or endometrial (uterine) curetting (scrapings of the endometrium with a spoon-shaped instrument). The tissue sample is then examined by your pathologist under the microscope. When viewed under the microscope, an endometrial polyp is made up of dilated endometrial glands and stroma with thick blood vessels.
Can cancer start in an endometrial polyp?
Very rarely, cancer will develop in an endometrial polyp. For this reason, your pathologist will examine the polyp for abnormal cells that may indicate the presence of a pre-cancerous condition called atypical endometrial hyperplasia or cancer. If any abnormal cells are seen, they will be described in your pathology report.
What are the types of endometrial polyps?
Some endometrial polyps look different when examined under a microscope. These polyps are called variants and are often given a special name that may be included in your report.
Some common variants include:
- Endometrial polyp with gland crowding – This is a polyp where the glands within the polyp are closer together than usual. This may require clinical follow-up and re-sampling of the endometrium to rule out a condition called endometrial hyperplasia.
- Adenomyomatous polyp – This type contains smooth muscle cells in addition to endometrial glands and stroma. It is a benign (non-cancerous) type of polyp.
- Mixed polyp – This type of polyp is made up of tissue from both the endometrium and a part of the cervix called the endocervix. For that reason, it has features of both an endometrial polyp and an endocervical polyp.
What is the recommended treatment for an endometrial polyp?
Most endometrial polyps can be successfully treated by surgery alone. However if your pathologist sees features that are worrisome (such as endometrial hyperplasia or cancer), your doctor may perform a procedure called a biopsy to look for changes in the tissue surrounding the polyp. For more information about treatment options, please talk to your doctor.


