by Catherine Forse MD FRCPC
January 17, 2024
Lymphocytic colitis is a pattern of injury caused by an increased number of immune cells within the mucosa that covers the inside surface of the colon. This leads to inflammation and damage which prevents the colon from functioning normally.
What are the symptoms of lymphocytic colitis?
People with lymphocytic colitis can develop watery diarrhea that can last from weeks to years. Other possible symptoms can include abdominal pain, weight loss, and fatigue. Lymphocytic colitis belongs to a group of related conditions called microscopic colitis. This group includes collagenous colitis which shares many features with lymphocytic colitis.
What causes lymphocytic colitis?
Doctors still do not know what causes a person to develop lymphocytic colitis in the first place. However, one theory suggests that it may be an autoimmune condition where immune cells start to attack the cells in the colon. Another theory suggests that the condition may be a reaction to material in fecal matter.
How is this diagnosis made?
If your doctor suspects lymphocytic colitis based on your symptoms, they will perform a colonoscopy. A colonoscopy is a procedure where a small camera is used to see the inside of your colon. During this procedure, your doctor will take tissue samples called biopsies. Because this condition can happen in one part of the colon but not another, they will likely take multiple biopsies from the entire length of the colon. Your pathologist will then examine these biopsies under a microscope to determine whether the features of lymphocytic colitis are present.
For most people with lymphocytic colitis, their colon will look entirely normal during the colonoscopy. That is because lymphocytic colitis is a ‘microscopic’ disease, and its features can only be seen when the tissue is examined under a microscope.
Microscopic features
When the tissue is examined under the microscope an increased number of specialized immune cells called lymphocytes are seen within the mucosa on the inside of the colon. These lymphocytes are seen both within the glands and the lamina propria. Pathologists describe this change as intraepithelial lymphocytosis.
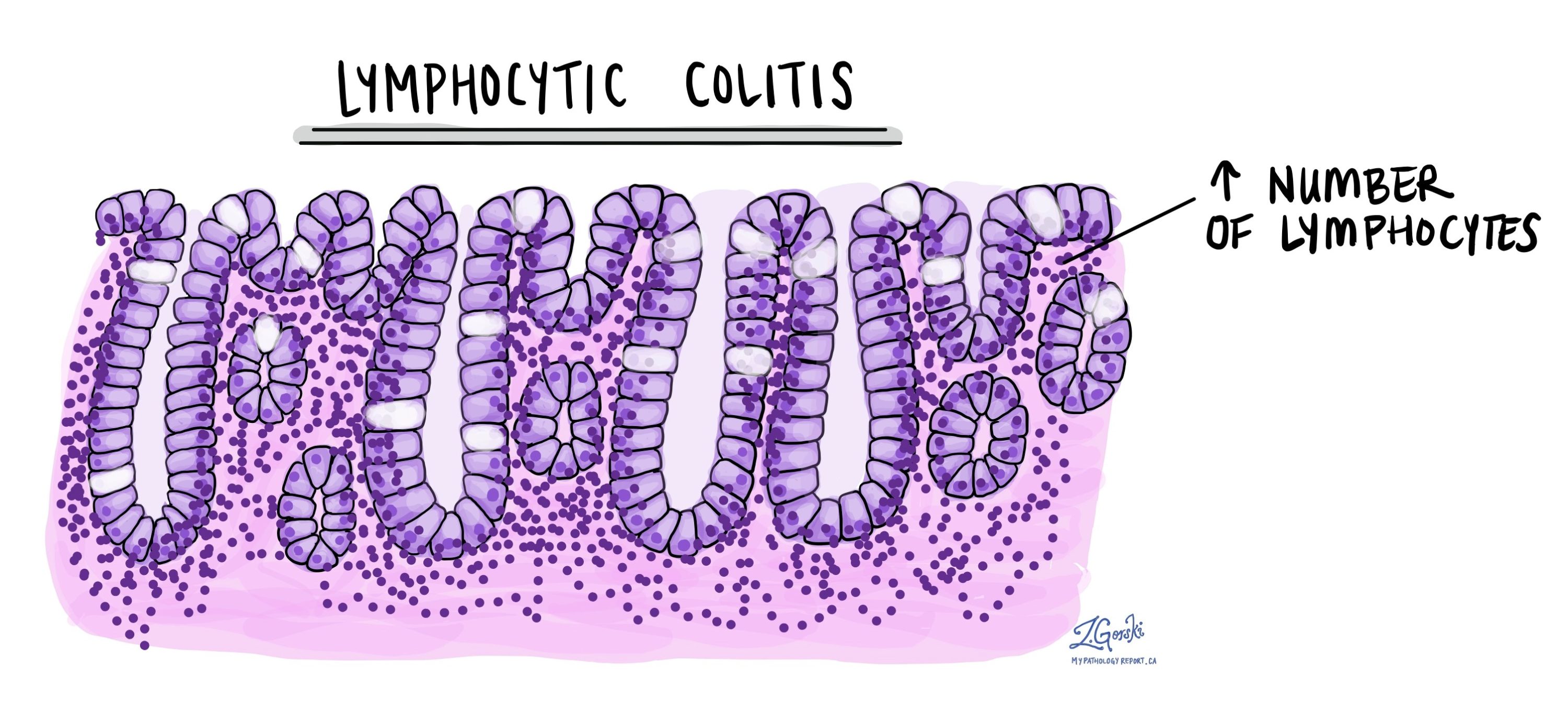
Over time, the increased lymphocytes damage the glands. This damage causes the cells to become smaller. Pathologists call this change atrophy. The smaller cells produce less mucin which prevents the colon from functioning normally.
While microscopic colitis can cause chronic inflammation in the colon, it is not the same as inflammatory bowel disease (IBD). IBD has many features which are not seen in microscopic colitis. For example, the size and shape of the crypts are abnormal. Pathologists call this change crypt distortion. To learn more about the features seen in IBD, read our article on chronic colitis.
About this article
This article was written by medical doctors in conjunction with patient advisers. It was designed to help patients read and understand their pathology report. If you have any questions about this article, please contact us.



