by Catherine Forse MD FRCPC
July 24, 2025
Collagenous colitis is a non-cancerous condition that causes inflammation and damage to the lining of the colon. It belongs to a group of conditions called microscopic colitis, named because the changes can only be seen when the tissue is examined under a microscope. The other main type of microscopic colitis is lymphocytic colitis, which shares many features with collagenous colitis.
What are the symptoms of collagenous colitis?
The most common symptom of collagenous colitis is chronic watery diarrhea that may last for weeks, months, or even years. Other symptoms may include:
-
Abdominal pain or cramping.
-
Bloating.
-
Fatigue.
-
Unintentional weight loss.
Some people experience symptoms that come and go, while others may have continuous symptoms that significantly affect daily life.
What causes collagenous colitis?
The exact cause of collagenous colitis is not fully understood. However, several factors may contribute:
-
Autoimmune reaction – Some researchers believe the immune system may mistakenly attack the cells lining the colon.
-
Medications – Certain drugs, including non-steroidal anti-inflammatory drugs (NSAIDs), proton pump inhibitors, and selective serotonin reuptake inhibitors (SSRIs), have been linked to the condition.
-
Infections or bacteria – Changes in the normal bacteria of the gut may trigger an abnormal immune response.
-
Genetics – Some people may have a genetic predisposition to developing microscopic colitis.
More research is needed to fully understand why collagenous colitis develops in some people and not others.
How is the diagnosis of collagenous colitis made?
If your doctor suspects collagenous colitis based on your symptoms, they will recommend a colonoscopy, a procedure that uses a small camera to look inside the colon. During the colonoscopy, your doctor will take small tissue samples called biopsies from different parts of the colon. This is important because the disease may affect only certain areas.
In most cases, the colon appears completely normal during the colonoscopy. That’s why the diagnosis can only be made when a pathologist examines the biopsies under a microscope.
What does collagenous colitis look like under the microscope?
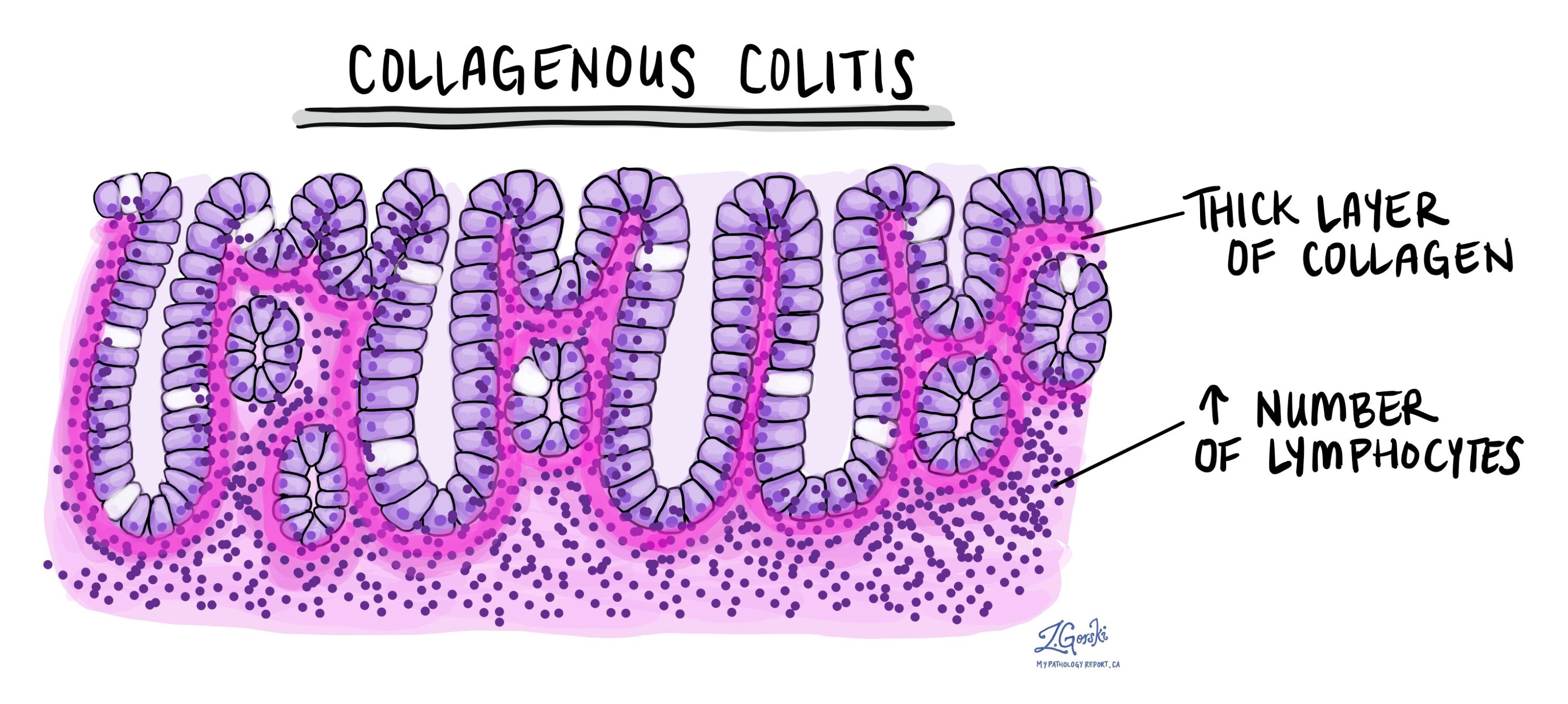
When viewed under the microscope, the tissue from the colon shows signs of inflammation and structural changes:
-
Intraepithelial lymphocytosis – An increased number of immune cells called lymphocytes are seen in the epithelial layer, the thin surface lining of the colon. These cells are also found in the lamina propria, the layer of tissue just beneath the epithelium.
-
Gland atrophy – The inflammation damages the glands (called crypts) that line the colon, causing them to shrink and produce less mucin. Mucin is a substance that helps protect and lubricate the colon.
-
Thickened collagen layer – A band of protein called collagen builds up just below the surface lining of the colon. This thickened layer is a defining feature of collagenous colitis and gives the condition its name. It often appears as a pink band when stained with special dyes like Masson’s trichrome.
-
Trapped blood vessels and immune cells – The thickened collagen layer can trap tiny blood vessels and immune cells close to the surface.
These microscopic changes interfere with how the colon normally absorbs water, leading to diarrhea.
Is collagenous colitis the same as inflammatory bowel disease (IBD)?
No, collagenous colitis is not the same as inflammatory bowel disease (IBD), which includes ulcerative colitis and Crohn’s disease. While both conditions involve inflammation in the colon, they have distinct microscopic features.
For example, in IBD:
-
The glands become distorted and irregular in shape, a change called crypt distortion.
-
Inflammation is often deeper and may involve the entire wall of the colon.
-
IBD can cause ulcers, abscesses, and long-term structural damage not typically seen in collagenous colitis.
Unlike IBD, collagenous colitis does not increase the risk of colon cancer, and it usually responds well to medications that reduce inflammation or change the immune response.
Questions to ask your doctor
-
Is my collagenous colitis mild, moderate, or severe?
-
What treatments are available, and do I need medication?
-
Should I avoid any specific medications that could worsen this condition?
-
Will I need regular follow-up or future colonoscopies?



