by Jason Wasserman MD PhD FRCPC and Zuzanna Gorski MD FRCPC
September 1, 2025
High grade squamous intraepithelial lesion (HSIL) is a precancerous condition of the cervix caused by human papillomavirus (HPV). It is made up of squamous cells that have been infected and changed by the virus. These abnormal cells are found in the transformation zone, which is the part of the cervix where glandular cells are replaced by squamous cells.

Another name for HSIL is cervical intraepithelial neoplasia, or CIN. CIN is divided into three levels based on severity: CIN1, CIN2, and CIN3. HSIL corresponds to CIN2 and CIN3, which are considered high grade changes.
Is high grade squamous intraepithelial lesion cancer?
HSIL is not cancer. However, it is considered a serious precancerous change because it increases the risk of developing a type of cervical cancer called HPV associated squamous cell carcinoma. Because of this risk, treatment is usually recommended to remove the abnormal cells before they can turn into cancer.
What is the risk of HSIL turning into cancer?
HSIL has a significant risk of progressing to cervical cancer if it is not treated. Studies show that without treatment, many cases of HSIL eventually develop into HPV associated squamous cell carcinoma. This is why treatment is almost always recommended once HSIL is confirmed.
The risk of progression is significantly higher than in low grade squamous intraepithelial lesion (LSIL), which often resolves on its own. By contrast, HSIL is less likely to resolve naturally and more likely to become persistent or progress. For this reason, monitoring alone is not typically considered a safe approach, and removing the abnormal cells is the standard method.
What is the difference between HSIL and LSIL?
Both HSIL and low grade squamous intraepithelial lesion (LSIL) are caused by HPV infection, but they behave differently. LSIL has a low risk of progressing to cancer and often resolves on its own without treatment. In contrast, HSIL is much more likely to progress to cancer if untreated, which is why active treatment is usually recommended.
What are the symptoms of HSIL?
Most people with HSIL do not experience any symptoms. This is why regular Pap tests and HPV screening are important for detecting changes early.
When symptoms do occur, they may include:
-
Abnormal vaginal bleeding, especially after sex or between periods.
-
Unusual vaginal discharge, which may be watery or tinged with blood.
-
Pelvic pain or discomfort, although this is less common.
Because HSIL rarely causes noticeable symptoms, most cases are found through routine cervical cancer screening.
What causes HSIL?
HSIL is caused by a persistent infection with high-risk types of HPV. HPV is a very common virus that spreads through skin-to-skin contact, including sexual contact. While most HPV infections are temporary and go away on their own, some infections persist in the cervix and cause abnormal changes in squamous cells.
The HPV types most often linked to HSIL and cervical cancer include HPV 16, 18, 31, 33, 51, and several others. These high-risk types can interfere with normal cell growth and survival, leading to precancerous changes.
Not everyone who is infected with HPV will develop HSIL. In many people, the immune system successfully clears the virus. However, some risk factors make HSIL more likely, including:
-
Persistent infection with high-risk HPV types.
-
A weakened immune system, which makes it harder to clear the virus.
-
Cigarette smoking, which makes cervical cells more vulnerable to HPV-related changes.
-
Long-term use of birth control pills.
-
Multiple sexual partners, which increases the risk of HPV exposure.
-
Lack of regular cervical screening.
How is the diagnosis of HSIL made?
HSIL is often first detected through a Pap test, which examines the cervix for abnormal squamous cells. If HSIL is suspected, further tests are performed to confirm the diagnosis and check for more advanced disease.
These tests may include:
-
HPV testing to check for high-risk HPV types.
-
Colposcopy, where the cervix is examined under magnification.
-
Cervical biopsy, in which a small piece of tissue is removed for microscopic examination.
-
Endocervical curettage, where cells are collected from the endocervical canal to look for hidden abnormal changes.
If a biopsy confirms HSIL, treatment is usually recommended to remove the abnormal cells.
What other tests may be performed?
Pathologists may use additional laboratory tests to confirm the diagnosis.
-
In situ hybridization can be used to detect HPV DNA or RNA inside the tumor cells. This test shows whether the abnormal cells are caused by high-risk HPV and can identify the specific HPV type.
-
Immunohistochemistry for p16 is often performed. HSIL cells almost always show strong block-like staining for p16, which supports the diagnosis and helps distinguish HSIL from LSIL or other conditions.
What does HSIL look like under the microscope?
When examined under the microscope, HSIL consists of squamous cells that are darker and larger than normal. These abnormal cells are confined to the epithelium, which is the surface lining of the cervix.
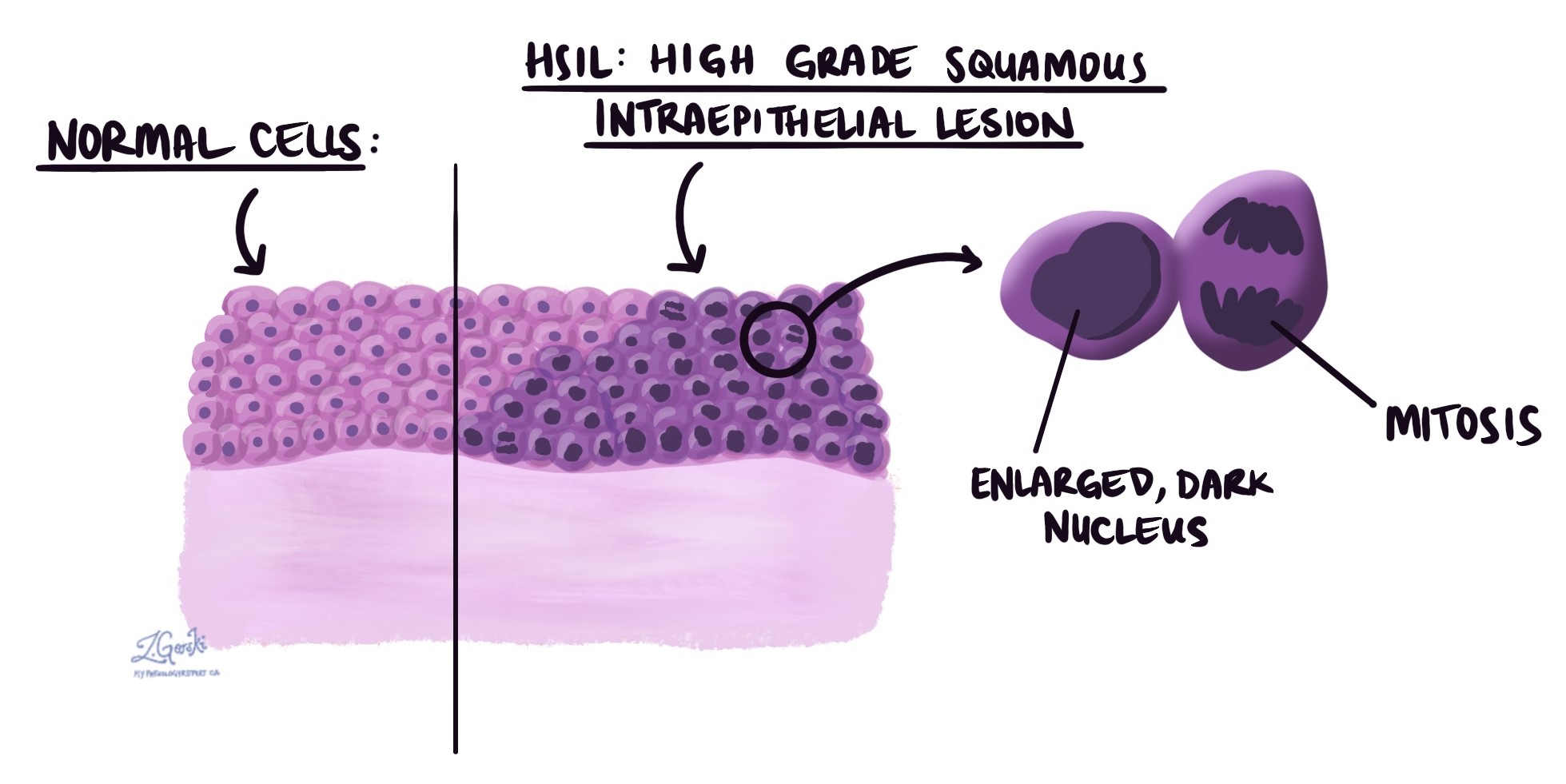
The cells are actively dividing, which is seen as many mitotic figures. These changes are a sign that the lesion is precancerous. Koilocytes, which are cells with irregular nuclei and clear spaces around them caused by HPV infection, may also be present, although they are more typical of LSIL.
What is the treatment for HSIL?
Treatment is usually recommended for HSIL to remove the abnormal cells and prevent the development of cervical cancer.
Common treatment options include:
-
Loop electrosurgical excision procedure (LEEP): A thin wire loop carrying an electrical current is used to remove the affected area of the cervix.
-
Cold knife cone biopsy (conization): A cone-shaped section of the cervix is surgically removed, usually in the operating room.
-
Cryotherapy: The abnormal tissue is destroyed by freezing.
-
Laser therapy: A focused laser beam is used to target and remove or destroy abnormal cells.
The choice of treatment depends on factors such as the size and location of the lesion, the patient’s age, and whether a future pregnancy is desired. After treatment, follow-up Pap tests and HPV testing are essential to make sure the lesion does not come back.
What happens after HSIL is diagnosed on a Pap test?
If HSIL is reported on a Pap test, your doctor will refer you for a colposcopy. If a biopsy confirms HSIL, treatment will usually be recommended. In some cases, if the affected area is very small, close monitoring with repeat testing may be considered, especially in younger women.
It is very important to attend all follow-up appointments. Untreated HSIL can progress to cervical cancer over time.
What are margins and why are they important?
Margins are the edges of the tissue removed during treatment. Pathologists examine the margins to see if any HSIL cells are present at the edge.
-
A negative margin means that no HSIL is present at the edge, which suggests that the lesion was removed entirely.
-
A positive margin means that HSIL cells are still present at the edge, which increases the risk that the lesion could return.
Margins are described in procedures such as LEEP and cone biopsy, but not in Pap smears or small biopsies. Different margins may be described, depending on which part of the cervix was removed. These include the endocervical margin (the inner part near the uterus), the ectocervical margin (the outer part near the vagina), and the stromal margin (the deeper tissue inside the cervix).
If HSIL is found at the margin, your doctor may recommend additional treatment or closer monitoring.
Questions to ask your doctor
-
Was HSIL the only finding on my Pap test or biopsy?
-
Did my sample test positive for high-risk HPV?
-
What treatment option do you recommend for me?
-
Will this treatment affect my ability to become pregnant in the future?
-
Were the margins clear after my treatment?
-
How often will I need follow-up Pap tests or HPV testing?
-
What is the chance that HSIL could come back?


