The pathologic stage of HPV associated endocervical adenocarcinoma is determined using the TNM staging system, an internationally recognized system created by the American Joint Committee on Cancer (AJCC).This system classifies the cancer based on:
- T (Tumour) – The size of the tumour and how far it has spread within the cervix and surrounding structures.
- N (Nodes) – Whether cancer cells are found in nearby lymph nodes.
- M (Metastasis) – Whether cancer has spread to distant parts of the body.
Your pathologist examines the tissue removed during surgery and assigns a stage to each category. Based on these findings, the overall stage is then determined. In general, a higher stage means a more advanced cancer that may require more aggressive treatment.
Tumour stage (pT) for HPV associated endocervical adenocarcinoma
The T stage describes how deeply the cancer has grown into the cervix and whether it has spread beyond it.
- T1a – The tumour is small and only detected under the microscope. It has grown no more than 5 millimetres deep and 7 millimetres wide.
- T1b – The tumour is large enough to be seen by the doctor during an exam or has grown deeper than 5 millimetres or wider than 7 millimetres.
- T2a – The tumour has spread beyond the cervix and uterus but has not invaded the parametrium (the connective tissue next to the cervix).
- T2b – The tumour has spread into the parametrium.
- T3a – The tumour has grown into the lower part of the vagina.
- T3b – The tumour has spread to the pelvic wall (the bony structure that encloses the reproductive organs) or has blocked the ureters, leading to kidney problems.
- T4 – The tumour has spread into the bladder or rectum or has extended beyond the pelvis into the abdomen.
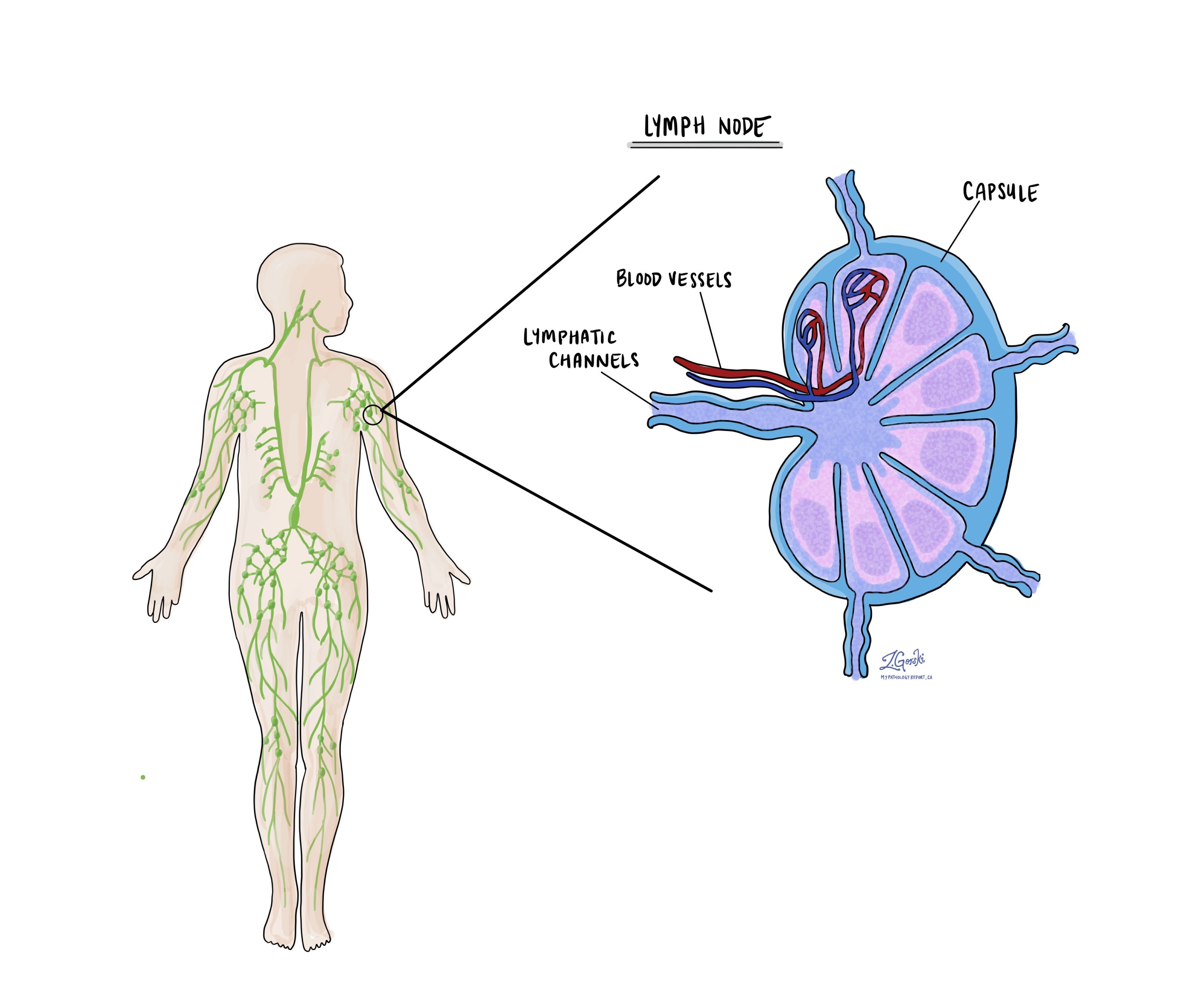
Nodal stage (pN) for HPV associated endocervical adenocarcinoma
The N stage describes whether cancer has spread to lymph nodes, small immune organs that help filter harmful substances. Lymph node involvement increases the risk that cancer may spread to other parts of the body.
- NX – No lymph nodes were removed for examination.
- N0 – No cancer cells were found in the lymph nodes.
- N0(i+) – Only isolated cancer cells (less than 0.2 millimetres in size) were found in a lymph node.
- N1 – A larger group of cancer cells (greater than 0.2 millimetres) was found in at least one lymph node.
The stage of the cancer plays a key role in determining the best treatment plan and predicting prognosis. Early-stage tumours (T1a, T1b) without lymph node involvement (N0) are typically treated with surgery alone, while more advanced stages (T2 and higher, or N1) may require additional treatments such as radiation or chemotherapy.
FIGO staging for HPV associated endocervical adenocarcinoma
The FIGO staging system is another method used to classify the extent of cervical cancer. FIGO, which stands for the International Federation of Gynecology and Obstetrics, developed this system specifically for cervical cancer. It is widely used by doctors to guide treatment decisions and predict outcomes. Unlike the TNM system, which considers tumour size, lymph node involvement, and metastasis separately, the FIGO system focuses on how far the cancer has spread beyond the cervix. Understanding the FIGO stage helps determine whether a patient may need surgery, radiation, chemotherapy, or a combination of treatments.
Stage I: Cancer is confined to the cervix
At this stage, the tumour has not spread beyond the cervix. The depth of invasion (how deep the tumour has grown into the cervix) is an important factor.
- Stage IA: Cancer is only visible under a microscope and has not formed a tumour that can be seen with the naked eye.
- Stage IA1: Cancer has grown 3 millimetres or less into the cervical tissue.
- Stage IA2: Cancer has grown between 3 and 5 millimetres into the cervical tissue.
- Stage IB: The tumour is larger than 5 millimetres and can be seen without a microscope but is still confined to the cervix.
- Stage IB1: Tumour is 2 centimetres or smaller.
- Stage IB2: Tumour is between 2 and 4 centimetres.
- Stage IB3: Tumour is larger than 4 centimetres.
Stage II: Cancer has spread beyond the cervix but not to the pelvic wall or lower third of the vagina
At this stage, the tumour has extended into nearby structures, but it has not reached the pelvic wall or lower vagina.
- Stage IIA: The cancer has spread to the upper two-thirds of the vagina but has not invaded the parametrium (the connective tissue next to the cervix).
- Stage IIA1: Tumour is 4 centimetres or smaller.
- Stage IIA2: Tumour is larger than 4 centimetres.
- Stage IIB: The tumour has spread into the parametrium (the tissues next to the cervix) but has not reached the pelvic wall.
Stage III: Cancer has spread to the lower third of the vagina, the pelvic wall, or nearby lymph nodes
At this stage, the tumour has extended further into surrounding structures.
- Stage IIIA: Cancer has spread to the lower third of the vagina but has not reached the pelvic wall.
- Stage IIIB: Cancer has spread to the pelvic wall or is blocking the ureters, which can cause kidney dysfunction.
- Stage IIIC: Cancer has spread to nearby lymph nodes, regardless of tumour size.
- Stage IIIC1: Cancer is found in pelvic lymph nodes only.
- Stage IIIC2: Cancer has spread to para-aortic lymph nodes (lymph nodes near the aorta in the abdomen).
Stage IV: Cancer has spread beyond the pelvis or to distant organs
Stage IV is the most advanced stage, meaning the cancer has spread beyond the pelvic region.
- Stage IVA: Cancer has spread to nearby organs, such as the bladder or rectum.
- Stage IVB: Cancer has spread to distant body parts, such as the lungs, liver, or bones.
Why is FIGO staging important for HPV associated endocervical adenocarcinoma?
FIGO staging helps doctors choose the best treatment plan and predict how the cancer may behave over time. Early-stage cancers (Stage I and some Stage II) are often treated with surgery alone, while more advanced stages (Stage IIIB and beyond) usually require a combination of radiation therapy and chemotherapy. The presence of lymph node involvement (Stage IIIC) is also important, as it increases the risk of cancer recurrence, which may lead to additional treatments. Your pathology report will include the FIGO stage, along with other important features such as tumour size, depth of invasion, lymph node involvement, and the presence of metastases. Your doctor will use this information to create a personalized treatment plan.
What is the prognosis for a person diagnosed with HPV associated endocervical adenocarcinoma?
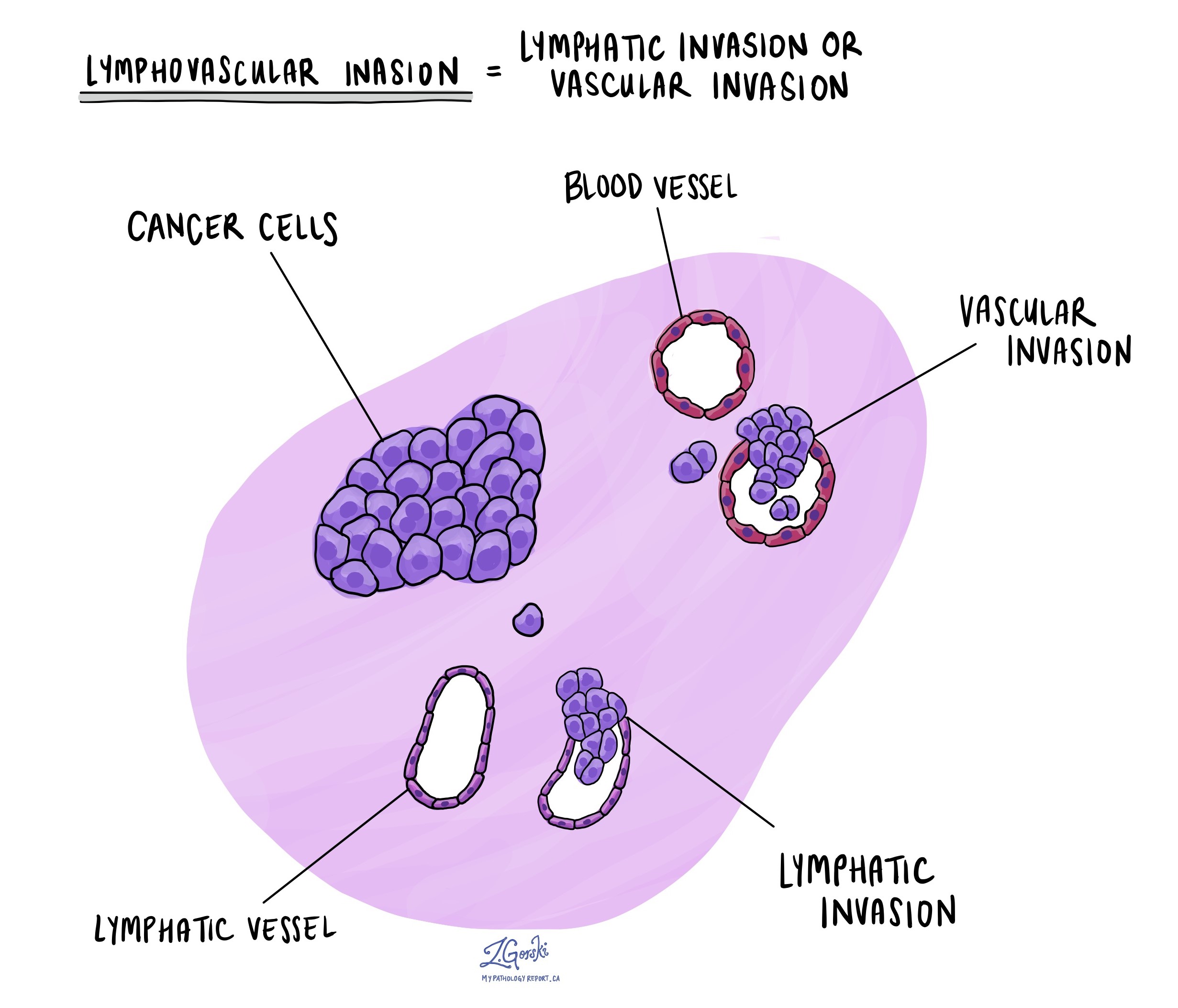
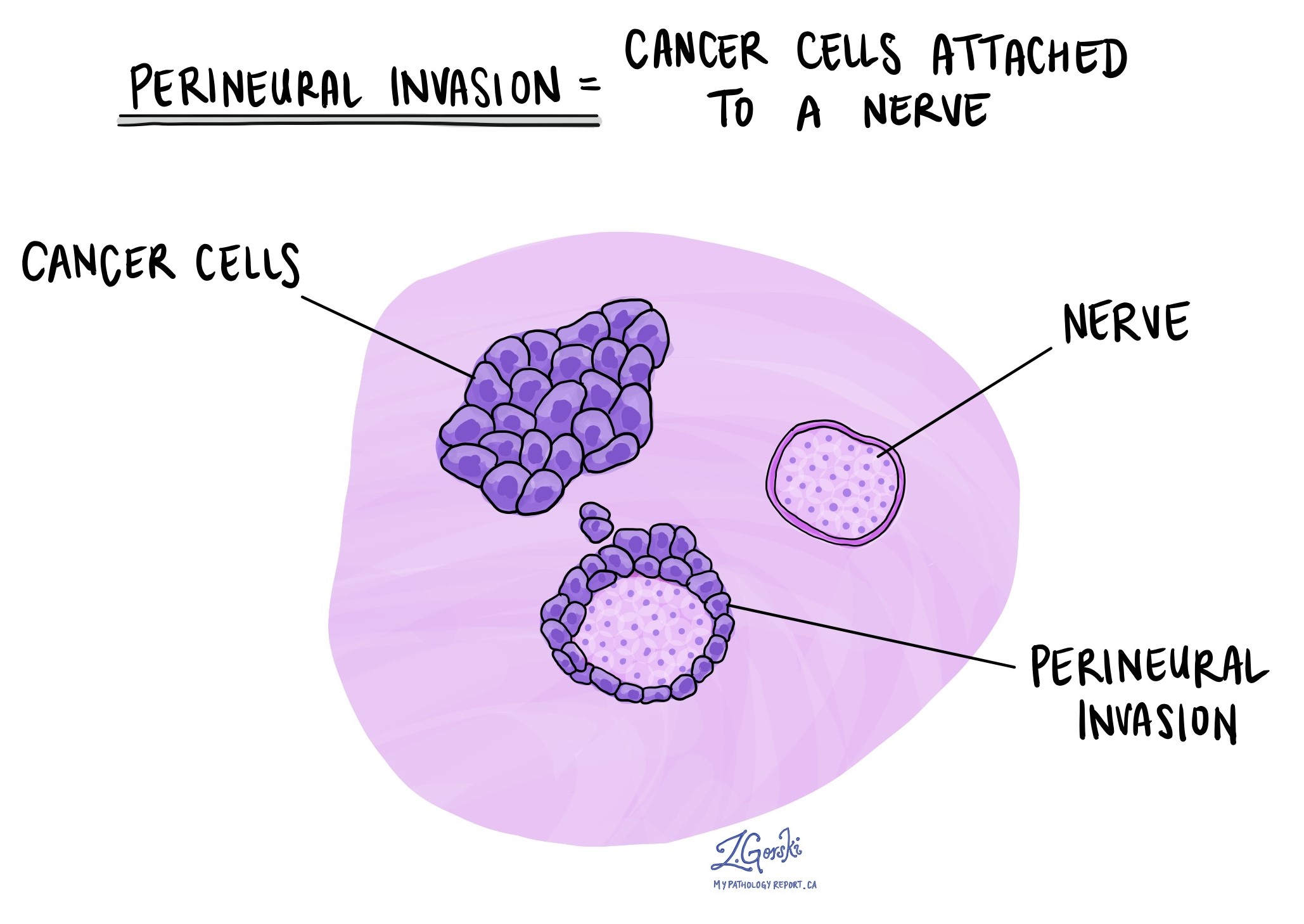
The prognosis for HPV associated endocervical adenocarcinoma depends on several factors, including the stage of the cancer at diagnosis, the pattern of invasion, the presence of lymphovascular invasion, and the patient’s overall health.
The stage of the cancer is the most important factor in determining prognosis. In early-stage disease, survival rates are very high. For example, patients with stage IA1 disease, which is the earliest stage, have nearly a 100% survival rate. For stage IA2, the survival rate is around 93%. However, as the cancer progresses, survival rates decrease significantly. For stage III disease, the survival rate drops to about 34%, and for stage IV, it is only 3%.
The Silva pattern of invasion also plays a significant role in prognosis. Tumours with Pattern A invasion, where the cancerous glands remain well-defined and do not invade destructively, have a very low risk of spreading to lymph nodes or recurring after treatment. In contrast, Pattern B and Pattern C tumours are more aggressive. Pattern B tumours, which show early or focal destructive invasion, have about a 4% risk of lymph node spread, while Pattern C tumours have a much higher risk of spread (around 25%). Among Pattern C tumours, those with micropapillary growth tend to have a greater risk of lymph node involvement. In comparison, tumours with diffuse destructive and confluent growth have a higher risk of recurrence and poorer survival outcomes.
Some genetic changes have been linked to prognosis. Mutations in the KRAS and PIK3CA genes are frequently found in HPV-associated endocervical adenocarcinomas, especially those with destructive invasion, and these mutations have been associated with a worse prognosis. However, overall, HPV-associated endocervical adenocarcinoma has a better prognosis than HPV independent endocervical adenocarcinoma, which is a different type of cervical cancer that is not caused by HPV.
Certain subtypes of HPV associated endocervical adenocarcinoma also have different prognoses. Villoglandular adenocarcinoma, a subtype that grows in finger-like projections, typically has an excellent prognosis as long as it remains confined to the cervix. However, if it invades deeply into the surrounding tissue, its behaviour becomes similar to that of other HPV associated adenocarcinomas. Some mucinous subtypes, such as stratified mucin-producing carcinoma, may have a worse prognosis compared to other HPV associated tumours.
For early-stage, non-destructively invasive tumours, conservative treatment with a cone biopsy (removal of part of the cervix) is often sufficient, and additional surgery is not needed. However, some studies have reported that even early-stage adenocarcinomas with an AIS-like appearance may, in rare cases, spread to the ovaries, meaning careful follow-up is required if a conservative treatment approach is chosen.
For more advanced tumours, treatment typically includes radical hysterectomy with lymph node removal and/or chemoradiation therapy. More aggressive treatment is often necessary if the tumour has lymphovascular invasion or is larger in size. Fertility-preserving options, such as radical trachelectomy (removal of the cervix while preserving the uterus), may be considered for stage IA tumours with lymphovascular invasion or for selected stage IB1 tumours, but only if lymph nodes remain cancer-free.Overall, the prognosis for HPV associated endocervical adenocarcinoma is good when diagnosed early, but survival decreases significantly if the cancer has spread beyond the cervix. Regular screening, early detection, and appropriate treatment are essential for improving outcomes.